Bradycardia Management Details
HRTD Medical Institute. Mobile Number 01969947171, 01797522136.Bradycardia management depends on whether the patient is stable or unstable, with unstable patients requiring immediate attention using atropine, followed by transcutaneous pacing, or epinephrine/dopamine infusions if atropine fails. Stable patients should be assessed for underlying causes, which might include medication adjustments, treating conditions like sleep apnea, or lifestyle changes. For persistent, severe cases, a permanent pacemaker may be required.
ব্র্যাডিকার্ডিয়া ব্যবস্থাপনা রোগীর স্থিতিশীলতা বা অস্থিরতার উপর নির্ভর করে। অস্থির রোগীদের তাৎক্ষণিক চিকিৎসার জন্য অ্যাট্রোপিন ব্যবহার করা হয়, তারপরে ট্রান্সকুটেনিয়াস পেসিং করা হয়, অথবা অ্যাট্রোপিন ব্যর্থ হলে এপিনেফ্রিন/ডোপামিন ইনফিউশন দেওয়া হয়। স্থিতিশীল রোগীদের অন্তর্নিহিত কারণগুলির জন্য মূল্যায়ন করা উচিত, যার মধ্যে ওষুধের সমন্বয়, স্লিপ অ্যাপনিয়ার মতো অবস্থার চিকিৎসা বা জীবনযাত্রার পরিবর্তন অন্তর্ভুক্ত থাকতে পারে। ক্রমাগত, গুরুতর ক্ষেত্রে, একটি স্থায়ী পেসমেকার প্রয়োজন হতে পারে।
Immediate Actions for Unstable Patients
- Assess for hemodynamic instability:Look for symptoms like shock, syncope (fainting), myocardial ischemia, or heart failure.
- Initiate support:Establish IV access, provide oxygen, and obtain continuous cardiac monitoring and a 12-lead ECG.
- Administer Atropine:A 1 mg bolus of IV atropine is given to increase heart rate. This dose can be repeated every 3 to 5 minutes, up to a maximum of 3 mg.
- Consider Transcutaneous Pacing:If atropine is ineffective, especially in unstable patients or during an acute MI, transcutaneous pacing can be initiated. Sedation and analgesia should be considered for conscious patients.
- Administer Inotropic Infusions:If pacing is not feasible or atropine is ineffective, use epinephrine or dopamine infusions to increase heart rate and support blood pressure.
Managing Stable Patients
- Identify the underlying cause:Investigate reversible causes such as electrolyte imbalances, sleep apnea, or systemic diseases like sarcoidosis.
- Adjust medications:Review and potentially adjust or stop medications that may be causing the bradycardia.
- Lifestyle changes:For some, healthy lifestyle modifications like regular exercise and a heart-healthy diet can be beneficial.
Long-Term Treatments
- Permanent Pacemaker: For patients with persistent, severe bradycardia or conditions like sick sinus syndrome where the heart’s natural pacemaker is not working, a permanent pacemaker may be the best long-term solution.
Diagnosis of Bradycardia
To diagnose bradycardia, a healthcare professional examines you and listens to your heart with a stethoscope. You are usually asked questions about your symptoms and medical history.
Tests
Tests may be done to check your heart and look for conditions that can cause bradycardia.
- Blood tests. A sample of your blood may be tested to check for infections and changes in body chemicals, such as potassium. A blood test also may be done to check thyroid function.
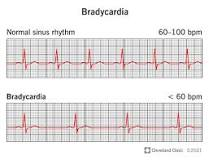
- Electrocardiogram (ECG or EKG). This is the main test used to diagnose bradycardia. An ECG measures the electrical activity of the heart. It shows how the heart is beating. Sticky patches with sensors are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which displays or prints the results.
- Holter monitor. If a standard ECG doesn’t show an irregular heartbeat, your healthcare professional may suggest a Holter monitor. This portable ECG device is worn for a day or more. It records the heart’s activity during daily activities.
- Event recorder. This device is similar to a Holter monitor, but it records only at certain times for a few minutes at a time. You typically press a button when symptoms occur. It’s worn for up to 30 days or until symptoms occur.
- Tilt table test. This test may be done if you’ve had fainting spells. A health professional checks your heart rate and blood pressure as you lie flat on a table. The table is tilted to put you in a standing position. The care professional watches how your heart and nervous system respond to the change in position.
- Stress exercise test. Some irregular heartbeats are triggered or made worse by exercise. During a stress test, the heart’s activity is watched while you ride on a stationary bicycle or walk on a treadmill. If you can’t exercise, you may be given medicine that affects the heart like exercise does.
- Sleep study. A sleep study may be suggested if you have repeated pauses in breathing during sleep, called obstructive sleep apnea. That condition may cause changes in the heartbeat.
Symptoms and Causes
Symptoms of bradycardia
For many people, bradycardia doesn’t cause any symptoms. This is especially true for people who are very physically active and have bradycardia because their hearts are more efficient. For people whose hearts can’t or don’t compensate, the symptoms tend to cause the following:
- Shortness of breath.
- Chest pain (angina).
- Fatigue.
- Heart palpitations (the unpleasant feeling of your own heartbeat without using your hands to feel for your pulse).
- Memory problems.
- Confusion.
- Difficulty concentrating.
- Dizziness, lightheadedness and fainting (syncope).
- Irritability, agitation or other personality changes.
These symptoms happen because of how bradycardia affects your heart and your brain.
Brain
The average human brain weighs about 3 pounds — about 1.6% of the total weight of a 180-pound person. Despite its small size, the brain gets between 15% and 20% of the blood that comes out of your heart. If there isn’t enough blood flow, that affects your brain function.
Heart
Bradycardia symptoms often look a lot like the symptoms of heart failure. Bradycardia can also look like angina, which is chest pain or pressure that’s a warning sign of heart disease.
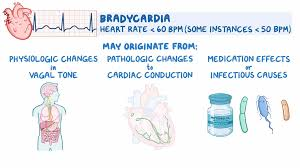
Causes of bradycardia
Bradycardia can happen for a wide range of reasons. Many of the other most common reasons include those listed below.
- Electrolyte deficiencies. Not getting enough of certain electrolytes like calcium, magnesium and potassium can impact your heart rate.
- Anorexia nervosa. This eating disorder is a potential cause of bradycardia.
- Inflammation. This includes inflammation of your heart’s inner lining (endocarditis), the heart muscle itself (myocarditis), or the pericardial sac that holds and cushions your heart (pericarditis).
- Infections. The bacteria that cause most strep throat infections can also cause damage to your heart, especially your heart valves if they aren’t treated quickly enough.
- Rheumatic fever and rheumatic heart disease. Rheumatic fever can develop when a bacterial infection like strep throat isn’t treated quickly. Rheumatic fever also causes rheumatic heart disease several years later.
- Lyme disease. This is a condition you get from bacteria that spread through tick bites. Also known as borreliosis, this condition can affect your heart if you go too long without treatment.
- Chagas disease. Similar to Lyme disease, this condition happens because of a parasite you can get from blood-sucking insects called “kissing bugs.”
- Sick sinus syndrome. This is when the heart’s natural pacemaker, a cluster of cells called the sinoatrial (SA) node, malfunctions. That means the SA node doesn’t correctly create the electrical current that travels through your heart and causes different parts to squeeze at the proper time.
- Heart block. This is a broad term that refers to any interruption in your heart’s electrical system. These interruptions block or slow down the electrical current as it travels, disrupting your heart’s beating process. Blocks can happen at many different points in your heart’s electrical conduction system.
- Drugs. These include prescription medications like beta-blockers, calcium-channel-blockers, anti-arrhythmia drugs, narcotic medications, lithium and depressants. Recreational drugs like cannabis (marijuana) can also cause bradycardia.
- Heart surgery. Repair of congenital heart conditions (meaning conditions that you’re born with), valve repair and valve replacement can all cause bradycardia.
- Radiation therapy. This treatment can cause toxic effects that lead to radiation heart disease.
Other conditions include:
- Heart attack.
- Heart failure.
- Coronary artery disease.
- Duchenne muscular dystrophy.
- Long Q-T syndrome.
- Lupus.
- Rheumatoid arthritis.
- Scleroderma.
- Injuries/trauma.
- Hypothermia (low body temperature).
- Hypothyroidism.
- Sleep apnea.
- Intracranial hypertension (too much pressure on your brain from swelling, bleeding or other causes).
 MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka
MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka