Orthopedic Diseases Details
Orthopedic Disease. Mobile Phone Number. 01797522136, 01987073965. Common Orthopedic Problems and Diseases are Low Back Pain, Muscle cramps, Osteoporosis, Osteoarthritis, Rheumatoid Arthritis, Ankylosing Spondylitis, Muscle atrophy, Bursitis, Knee pain, Frozen shoulder, Shoulder arthritis, Dislocated shoulder,

Fibromyalgia, Ankle sprains, Fracture, Carpal tunnel syndrome, Acute injuries, Musculoskeletal cancer, Hip labral tear, Tennis elbow, Rotator cuff tear, Anterior cruciate ligament injury, Scoliosis, Rickets, Gout, etc. You can study Orthopedic Disease in PDT Orthopedic Courses. These courses are PDT Orthopedics 6 Months, PDT Orthopedics 1 Year, and PDT Orthopedics 2 Years. All these courses are available at HRTD Medical Institute.
Students can study PDT Orthopedic Courses after completing the Diploma Medical Courses of Long and Short Duration. Diploma Medical Courses are DMF, DMA 3 Years, DMA 2 Years, DMA 1 Year, DMS 3 Years, DMS 2 Years, DMS 1 Year, DMDS 4 Years, etc. All the Diploma Courses are available at HRTD Medical Institute. You must have a science background for the DMF course and any background (But minimum SSC Pass) for other medical diploma courses.
Low Back Pain
Pain in the lower part of the back is called low back pain.
পিঠের নিচের অংশের ব্যথাকে লো ব্যাক পেইন বলে
Causes of Low back pain
A sprain is a common orthopedic disease. A sprain is a soft tissue injury of the ligaments within a joint, often caused by a sudden movement abruptly forcing the joint to exceed its functional range of motion
মোচ একটি সাধারণ অর্থোপেডিক রোগ। মোচ হল একটি জয়েন্টের অভ্যন্তরে লিগামেন্টের নরম টিস্যুতে আঘাত, প্রায়শই হঠাৎ নড়াচড়ার কারণে জয়েন্টটিকে তার কার্যকরী গতির সীমা ছাড়িয়ে যেতে বাধ্য করে।
Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with leaning forward
স্পাইনাল স্টেনোসিস হল স্পাইনাল ক্যানেল বা নিউরাল ফোরামেনের অস্বাভাবিক সংকীর্ণতা যার ফলে মেরুদন্ড বা স্নায়ুর শিকড়ের উপর চাপ পড়ে। লক্ষণগুলির মধ্যে বাহু বা পায়ে ব্যথা, অসাড়তা বা দুর্বলতা অন্তর্ভুক্ত থাকতে পারে। লক্ষণগুলি সাধারণত ধীরে ধীরে শুরু হয় এবং সামনের দিকে ঝুঁকে উন্নতি হয়
The most common orthopedic disease in elderly persons. Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to more porous bone, and a consequent increase in fracture risk. It is the most common reason for a broken bone among the elderly.
বয়স্ক ব্যক্তিদের মধ্যে সবচেয়ে সাধারণ অর্থোপেডিক রোগ। অস্টিওপোরোসিস হল একটি সিস্টেমিক কঙ্কালের ব্যাধি যা কম হাড়ের ভর, হাড়ের টিস্যুর মাইক্রো-আর্কিটেকচারাল অবনতি যা আরও ছিদ্রযুক্ত হাড়ের দিকে পরিচালিত করে এবং এর ফলে ফ্র্যাকচারের ঝুঁকি বৃদ্ধি পায়। এটি বয়স্কদের মধ্যে হাড় ভাঙ্গার সবচেয়ে সাধারণ কারণ
Osteoarthritis is an orthopedic disease. Osteoarthritis is a type of degenerative joint disease that results from the breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness.
Spinal stenosis
Osteoarthritis
Herniated disk
A herniated, or bulging, disc is a disc that has “spilled out” of its lining. This happens most frequently in the lower back.
অস্টিওআর্থারাইটিস একটি অর্থোপেডিক রোগ। অস্টিওআর্থারাইটিস হল এক ধরনের ডিজেনারেটিভ জয়েন্ট ডিজিজ যা জয়েন্ট কার্টিলেজ এবং অন্তর্নিহিত হাড় ভেঙে যাওয়ার ফলে হয়। এটি বিশ্বে অক্ষমতার চতুর্থ প্রধান কারণ বলে মনে করা হয়, যা শুধুমাত্র মার্কিন যুক্তরাষ্ট্রে প্রতি 7 জনের মধ্যে 1 জন প্রাপ্তবয়স্ককে প্রভাবিত করে। সবচেয়ে সাধারণ লক্ষণ হল জয়েন্টে ব্যথা এবং শক্ত হওয়া।
- স্পাইনাল স্টেনোসিস
- অস্টিওআর্থারাইটিস
- হার্নিয়েটেড ডিস্ক
- হার্নিয়েটেড ডিস্ক
একটি হার্নিয়েটেড, বা বুলিং, ডিস্ক হল একটি ডিস্ক যা এর আস্তরণের “ছিটকে গেছে”। এটি পিঠের নীচের অংশে প্রায়শই ঘটে।
Scoliosis is a condition in which a person’s spine has an irregular curve. The curve is usually S-shaped when viewed from the side.
স্কোলিওসিস এমন একটি অবস্থা যেখানে একজন ব্যক্তির মেরুদণ্ডে একটি অনিয়মিত বক্ররেখা থাকে। পাশ থেকে দেখা হলে বক্ররেখা সাধারণত S-আকৃতির হয়।
Osteoporosis
The most common orthopedic disease in elderly persons. Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to more porous bone, and a consequent increase in fracture risk. It is the most common reason for a broken bone among the elderly.
বয়স্ক ব্যক্তিদের মধ্যে সবচেয়ে সাধারণ অর্থোপেডিক রোগ। অস্টিওপোরোসিস হল একটি সিস্টেমিক কঙ্কালের ব্যাধি যা কম হাড়ের ভর, হাড়ের টিস্যুর মাইক্রো-আর্কিটেকচারাল অবনতি যা আরও ছিদ্রযুক্ত হাড়ের দিকে পরিচালিত করে এবং এর ফলে ফ্র্যাকচারের ঝুঁকি বৃদ্ধি পায়। এটি বয়স্কদের মধ্যে হাড় ভাঙ্গার সবচেয়ে সাধারণ কারণ।
Causes of Osteoporosis
Osteoporosis is a common orthopedic disease. Osteoporosis occurs when too much bone mass is lost and changes occur in the structure of bone tissue.
Bone is a living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Certain risk factors may lead to the development of osteoporosis.
Sex. Women have a greater risk for osteoporosis than men.
Age. As you age, bone loss happens more quickly, and new bone growth is slower.
Body size. Slender, thin-boned women and men are at greater risk of developing osteoporosis.
Skin Condition. White skin is at the highest risk.
Family history. The risk for osteoporosis and fractures may increase if one of your parents has a history of osteoporosis.
Changes to hormones. Low levels of certain hormones can increase osteoporosis. For example:
Low levels of estrogen in women ( during menopause).
Low levels of testosterone in men.
Diet. A diet low in calcium and vitamin D can increase your risk for osteoporosis and fractures.
Excessive dieting or poor protein intake may increase the risk for bone loss and osteoporosis.
Other medical conditions. Endocrine and hormonal diseases, gastrointestinal diseases, rheumatoid arthritis, certain types of cancer, HIV/AIDS, and anorexia nervosa.
Medications. Long-term use of certain medications:
Glucocorticoids and adrenocorticotropic hormone.
Antiepileptic medicines.
Cancer medications.
Proton pump inhibitors.
Selective serotonin reuptake inhibitors.
Thiazolidinediones, which treat type II diabetes.
Lifestyle.Low levels of physical activity.
Chronic heavy drinking of alcohol is a significant risk factor for osteoporosis.
অস্টিওপোরোসিসের কারণ
অস্টিওপোরোসিস একটি সাধারণ অর্থোপেডিক রোগ। অস্টিওপোরোসিস ঘটে যখন খুব বেশি হাড়ের ভর হারিয়ে যায় এবং হাড়ের টিস্যুর গঠনে পরিবর্তন ঘটে।
হাড় একটি জীবন্ত টিস্যু যা ক্রমাগত ভেঙ্গে এবং প্রতিস্থাপিত হয়। অস্টিওপোরোসিস ঘটে যখন নতুন হাড়ের সৃষ্টি পুরানো হাড়ের ক্ষতির সাথে তাল মিলিয়ে না যায়।
কিছু ঝুঁকির কারণ অস্টিওপরোসিসের বিকাশ ঘটাতে পারে।
সেক্স। পুরুষদের তুলনায় মহিলাদের অস্টিওপরোসিসের ঝুঁকি বেশি।
বয়স। আপনার বয়স বাড়ার সাথে সাথে হাড়ের ক্ষয় আরও দ্রুত হয় এবং নতুন হাড়ের বৃদ্ধি ধীর হয়।
শরীরের আকার। সরু, পাতলা হাড়যুক্ত মহিলা এবং পুরুষদের অস্টিওপোরোসিস হওয়ার ঝুঁকি বেশি।
ত্বকের অবস্থা। সাদা চামড়া সবচেয়ে বেশি ঝুঁকিতে থাকে।
পারিবারিক ইতিহাস। আপনার পিতামাতার একজনের অস্টিওপরোসিসের ইতিহাস থাকলে অস্টিওপোরোসিস এবং ফ্র্যাকচারের ঝুঁকি বাড়তে পারে।
হরমোনের পরিবর্তন। নির্দিষ্ট হরমোনের কম মাত্রা অস্টিওপরোসিস বাড়াতে পারে। যেমন:
মহিলাদের মধ্যে ইস্ট্রোজেনের নিম্ন স্তর (মেনোপজের সময়)।
পুরুষদের মধ্যে টেসটোসটেরনের মাত্রা কম।
ডায়েট। ক্যালসিয়াম এবং ভিটামিন ডি কম খাবার অস্টিওপরোসিস এবং ফ্র্যাকচারের ঝুঁকি বাড়াতে পারে।
অত্যধিক ডায়েটিং বা দুর্বল প্রোটিন গ্রহণ হাড় ক্ষয় এবং অস্টিওপরোসিসের ঝুঁকি বাড়াতে পারে।
অন্যান্য চিকিৎসা শর্ত। এন্ডোক্রাইন এবং হরমোনজনিত রোগ, গ্যাস্ট্রোইনটেস্টাইনাল রোগ, রিউমাটয়েড আর্থ্রাইটিস, নির্দিষ্ট ধরনের ক্যান্সার, এইচআইভি/এইডস এবং অ্যানোরেক্সিয়া নার্ভোসা।
ওষুধ। নির্দিষ্ট ওষুধের দীর্ঘমেয়াদী ব্যবহার:
Glucocorticoids এবং adrenocorticotropic হরমোন।
এন্টিপিলেপটিক ওষুধ।
ক্যান্সারের ওষুধ।
প্রোটন পাম্প ইনহিবিটার।
নির্বাচনী সেরোটোনিন রিউপটেক ইনহিবিটার।
থিয়াজোলিডিনিডিওনস, যা টাইপ II ডায়াবেটিসের চিকিত্সা করে।
জীবনধারা।নিম্ন মাত্রার শারীরিক কার্যকলাপ।
দীর্ঘস্থায়ী মদ্যপান অস্টিওপরোসিসের জন্য একটি উল্লেখযোগ্য ঝুঁকির কারণ।
Clinical features of Osteoporosis
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain is caused by a broken or collapsed bone in the spine.
- Loss of height over time.
- A stooped posture.
- A bone that breaks much more easily than expected. When to see a doctor
You might want to talk to your healthcare provider about osteoporosis if you went through early menopause or took corticosteroids for several months at a time, or if either of your parents had hip fractures.
অস্টিওপোরোসিসের ক্লিনিকাল বৈশিষ্ট্য
হাড় ক্ষয়ের প্রাথমিক পর্যায়ে সাধারণত কোন উপসর্গ থাকে না। কিন্তু একবার আপনার হাড়গুলি অস্টিওপোরোসিস দ্বারা দুর্বল হয়ে গেলে, আপনার লক্ষণ এবং উপসর্গ থাকতে পারে যার মধ্যে রয়েছে:
- মেরুদণ্ডের হাড় ভেঙে যাওয়া বা ভেঙে যাওয়ায় পিঠে ব্যথা হয়।
- সময়ের সাথে সাথে উচ্চতা হ্রাস।
- একটি স্তব্ধ ভঙ্গি.
- একটি হাড় যা প্রত্যাশার চেয়ে অনেক বেশি সহজে ভেঙে যায়। কখন ডাক্তার দেখাবেন
আপনি আপনার স্বাস্থ্যসেবা প্রদানকারীর সাথে অস্টিওপোরোসিস সম্পর্কে কথা বলতে চাইতে পারেন যদি আপনি প্রাথমিক মেনোপজের মধ্য দিয়ে যান বা এক সময়ে কয়েক মাস কর্টিকোস্টেরয়েড গ্রহণ করেন, বা আপনার পিতামাতার কারোর নিতম্বের ফাটল থাকে।
Risk factors
Many factors can increase the likelihood that you’ll develop osteoporosis — including your age, race, lifestyle choices, and medical conditions and treatments.
Unchangeable risks
Some risk factors for osteoporosis are out of your control, including:
- Your sex. Women are much more likely to develop osteoporosis than are men.
- Age. The older you get, the greater your risk of osteoporosis.
- Race. You’re at greatest risk of osteoporosis if you’re white or of Asian descent.
- Family history. Having a parent or sibling with osteoporosis puts you at greater risk, especially if your mother or father fractured a hip.
- Body frame size. Men and women who have small body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
অনেক কারণ আপনার অস্টিওপরোসিস হওয়ার সম্ভাবনা বাড়িয়ে দিতে পারে — আপনার বয়স, জাতি, জীবনধারা পছন্দ, এবং চিকিৎসা পরিস্থিতি এবং চিকিত্সা সহ।
অপরিবর্তনীয় ঝুঁকি
অস্টিওপরোসিসের কিছু ঝুঁকির কারণ আপনার নিয়ন্ত্রণের বাইরে, যার মধ্যে রয়েছে:
Your Sex: পুরুষদের তুলনায় মহিলাদের অস্টিওপরোসিস হওয়ার সম্ভাবনা অনেক বেশি।
Age: আপনার বয়স যত বেশি হবে, অস্টিওপরোসিসের ঝুঁকি তত বেশি হবে।
Race: আপনি যদি সাদা বা এশিয়ান বংশোদ্ভূত হন তাহলে আপনার অস্টিওপরোসিসের সবচেয়ে বেশি ঝুঁকি রয়েছে।
Family history: অস্টিওপোরোসিসে আক্রান্ত পিতা-মাতা বা ভাইবোন থাকা আপনাকে আরও ঝুঁকির মধ্যে ফেলে, বিশেষ করে যদি আপনার মা বা বাবার নিতম্ব ভেঙে যায়।
Body frame size: যে সমস্ত পুরুষ এবং মহিলাদের শরীরের ফ্রেমগুলি ছোট তাদের ঝুঁকি বেশি থাকে কারণ বয়সের সাথে সাথে তাদের হাড়ের ভর কম হতে পারে।
Hormone levels
Osteoporosis is more common in people who have too much or too little of certain hormones in their bodies. Examples include:
হরমোনের মাত্রা
অস্টিওপোরোসিস এমন লোকদের মধ্যে বেশি দেখা যায় যাদের শরীরে নির্দিষ্ট হরমোন খুব বেশি বা খুব কম থাকে। উদাহরণ অন্তর্ভুক্ত
- Sex hormones. Lowered sex hormone levels tend to weaken bones. The fall in estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis. Treatments for prostate cancer that reduce testosterone
- সেক্স হরমোন। যৌন হরমোনের মাত্রা কমে গেলে হাড় দুর্বল হয়ে যায়। মেনোপজের সময় মহিলাদের মধ্যে ইস্ট্রোজেনের মাত্রা কমে যাওয়া অস্টিওপরোসিস হওয়ার জন্য সবচেয়ে শক্তিশালী ঝুঁকির কারণগুলির মধ্যে একটি। প্রোস্টেট ক্যান্সারের চিকিৎসা যা টেস্টোস্টেরন কমায়
levels in men and treatments for breast cancer that reduce estrogen levels in women are likely to accelerate bone loss.
পুরুষদের মধ্যে মাত্রা এবং স্তন ক্যান্সারের চিকিত্সা যা মহিলাদের মধ্যে ইস্ট্রোজেনের মাত্রা হ্রাস করে তা হাড়ের ক্ষয়কে ত্বরান্বিত করতে পারে।
- Thyroid problems. Too much thyroid hormone can cause bone loss. This can occur if your thyroid is overactive or if you take too much thyroid hormone medicine to treat an underactive thyroid.
- থাইরয়েড সমস্যা: অত্যধিক থাইরয়েড হরমোন হাড় ক্ষয় হতে পারে। এটি ঘটতে পারে যদি আপনার থাইরয়েড অত্যধিক সক্রিয় হয় বা যদি আপনি একটি কম থাইরয়েডের চিকিত্সার জন্য খুব বেশি থাইরয়েড হরমোনের ওষুধ খান।
- Other glands. Osteoporosis has also been associated with overactive parathyroid and adrenal glands. Dietary factors
- অন্যান্য গ্রন্থি: অস্টিওপোরোসিস অতিরিক্ত সক্রিয় প্যারাথাইরয়েড এবং অ্যাড্রিনাল গ্রন্থির সাথেও যুক্ত। খাদ্যতালিকাগত কারণ
Osteoporosis is more likely to occur in people who have:
- Low calcium intake. A lifelong lack of calcium plays a role in the development of osteoporosis. Low calcium intake contributes to diminished bone density, early bone loss, and an increased risk of fractures.
- Low calcium intake.ক্যালসিয়ামের আজীবন অভাব অস্টিওপরোসিসের বিকাশে ভূমিকা পালন করে। কম ক্যালসিয়াম গ্রহণ হাড়ের ঘনত্ব হ্রাস, হাড়ের তাড়াতাড়ি ক্ষয় এবং ফ্র্যাকচারের ঝুঁকি বাড়ায়।
- Eating disorders. Severely restricting food intake and being underweight weaken bone in both men and women.
- Eating disorders.খাদ্য গ্রহণে কঠোরভাবে সীমাবদ্ধতা এবং কম ওজন নারী ও পুরুষ উভয়ের হাড়কে দুর্বল করে দেয়।
- Gastrointestinal surgery. Surgery to reduce the size of your stomach or to remove part of the intestine limits the amount of surface area available to absorb nutrients, including calcium. These surgeries include those to help you lose weight and other gastrointestinal disorders.
- Gastrointestinal surgery. আপনার পেটের আকার কমাতে বা অন্ত্রের অংশ অপসারণ করার জন্য সার্জারি ক্যালসিয়াম সহ পুষ্টি শোষণের জন্য উপলব্ধ পৃষ্ঠ এলাকার পরিমাণকে সীমিত করে। এই সার্জারিগুলির মধ্যে রয়েছে যা আপনাকে ওজন কমাতে সাহায্য করে এবং অন্যান্য গ্যাস্ট্রোইনটেস্টাইনাল ব্যাধি।
Steroids and other medicines
Long-term use of oral or injected corticosteroid medicines, such as prednisone and cortisone, interferes with the bone-rebuilding process. Osteoporosis has also been associated with medications used to combat or prevent:
প্রিডনিসোন এবং কর্টিসোনের মতো মৌখিক বা ইনজেকশনযুক্ত কর্টিকোস্টেরয়েড ওষুধের দীর্ঘমেয়াদী ব্যবহার হাড়ের পুনর্গঠন প্রক্রিয়াতে হস্তক্ষেপ করে। অস্টিওপোরোসিস প্রতিরোধ বা প্রতিরোধের জন্য ব্যবহৃত ওষুধের সাথেও যুক্ত করা হয়েছে:
- Seizures.
- Gastric reflux.
- Cancer.
- Transplant rejection.
- খিঁচুনি।
- গ্যাস্ট্রিক রিফ্লাক্স।
- ক্যান্সার।
- ট্রান্সপ্লান্ট প্রত্যাখ্যান।
Medical problems
The risk of osteoporosis is higher in people who have certain medical problems, including:
- Celiac disease.
- Inflammatory bowel disease.
- Kidney or liver disease.
- Cancer.
- Multiple myeloma.
- Rheumatoid arthritis. Lifestyle choices
- সিলিয়াক রোগ।
- প্রদাহজনক অন্ত্রের রোগ।
- কিডনি বা লিভারের রোগ।
- ক্যান্সার।
- একাধিক মায়োলোমা।
- রিউমাটয়েড আর্থ্রাইটিস। জীবনধারা পছন্দ
Some bad habits can increase your risk of osteoporosis. Examples include:
- Sedentary lifestyle. People who spend a lot of time sitting have a higher risk of osteoporosis than do those who are more active. Any weight-bearing exercise and activities that promote balance and good posture are good for your bones, but walking, running, jumping, dancing and weightlifting seem particularly helpful.
- Sedentary lifestyle. যারা বেশি সময় বসে থাকেন তাদের অস্টিওপরোসিসের ঝুঁকি বেশি থাকে যারা বেশি সক্রিয় তাদের তুলনায়। যেকোন ওজন বহন করার ব্যায়াম এবং ক্রিয়াকলাপ যা ভারসাম্য এবং ভাল অঙ্গবিন্যাস বাড়ায় আপনার হাড়ের জন্য ভাল, তবে হাঁটা, দৌড়ানো, লাফ দেওয়া, নাচ এবং ভারোত্তোলন বিশেষভাবে সহায়ক বলে মনে হয়।
- Excessive alcohol consumption. Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis.
- Excessive alcohol consumption.দিনে দুটির বেশি অ্যালকোহলযুক্ত পানীয় নিয়মিত সেবন অস্টিওপোরোসিসের ঝুঁকি বাড়ায়।
- Tobacco use. The exact role tobacco plays in osteoporosis isn’t clear, but it has been shown that tobacco use contributes to weak bones.
- Tobacco use. অস্টিওপোরোসিসে তামাক কী ভূমিকা পালন করে তা স্পষ্ট নয়, তবে এটি দেখানো হয়েছে যে তামাক ব্যবহার দুর্বল হাড়গুলিতে অবদান রাখে।
Complications
Compression fractures
Bone breaks, particularly in the spine or hip, are the most serious complications of osteoporosis. Hip fractures often are caused by a fall and can result in disability and even an increased risk of death within the first year after the injury.
In some cases, broken bones in the spine can occur even if you haven’t fallen. The bones that make up your spine, called vertebrae, can weaken to the point of collapsing, which can result in back pain, lost height, and a hunched-forward posture.
হাড় ভাঙ্গা, বিশেষ করে মেরুদণ্ড বা নিতম্বে, অস্টিওপোরোসিসের সবচেয়ে গুরুতর জটিলতা। নিতম্বের ফাটল প্রায়ই পড়ে যাওয়ার কারণে হয় এবং এর ফলে অক্ষমতা এবং এমনকি আঘাতের পর প্রথম বছরের মধ্যে মৃত্যুর ঝুঁকিও বেড়ে যায়।
কিছু ক্ষেত্রে, মেরুদণ্ডের হাড় ভাঙা এমনকি যদি আপনি পড়ে না থাকেন। আপনার মেরুদণ্ড তৈরি করা হাড়গুলি, যাকে কশেরুকা বলা হয়, ভেঙ্গে যাওয়ার পর্যায়ে দুর্বল হয়ে যেতে পারে, যার ফলে পিঠে ব্যথা, উচ্চতা হারানো এবং একটি কুঁকড়ে যাওয়া ভঙ্গি হতে পারে।
Prevention
Good nutrition and regular exercise are essential for keeping your bones healthy throughout your life.
ভাল পুষ্টি এবং নিয়মিত ব্যায়াম আপনার সারা জীবন আপনার হাড় সুস্থ রাখার জন্য অপরিহার্য।
Calcium
Men and women between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn 50 and men turn 70.
18 থেকে 50 বছর বয়সী পুরুষ এবং মহিলাদের প্রতিদিন 1,000 মিলিগ্রাম ক্যালসিয়াম প্রয়োজন। এই দৈনিক পরিমাণ 1,200 মিলিগ্রামে বৃদ্ধি পায় যখন মহিলারা 50 এবং পুরুষদের 70 বছর বয়সে পরিণত হয়।
Good sources of calcium include:
- Low-fat dairy products.
- Dark green leafy vegetables.
- Canned salmon or sardines with bones.
- Soy products, such as tofu.
- Calcium-fortified cereals and orange juice.
- কম চর্বিযুক্ত দুগ্ধজাত পণ্য।
- গাঢ় সবুজ শাক।
- হাড় সহ টিনজাত সালমন বা সার্ডিন।
- সয়া পণ্য, যেমন টফু।
- ক্যালসিয়াম-ফোর্টিফাইড সিরিয়াল এবং কমলার রস।
If you find it difficult to get enough calcium from your diet, consider taking calcium supplements. However, too much calcium has been linked to kidney stones. Although yet unclear, some experts suggest that too much calcium, especially in supplements, can increase the risk of heart disease.
The Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine recommends that total calcium intake, from supplements and diet combined, should be no more than 2,000 milligrams daily for people older than 50.
আপনার খাদ্য থেকে পর্যাপ্ত ক্যালসিয়াম পাওয়া কঠিন মনে হলে ক্যালসিয়াম সম্পূরক গ্রহণের কথা বিবেচনা করুন। যাইহোক, অত্যধিক ক্যালসিয়াম কিডনি পাথরের সাথে যুক্ত করা হয়েছে। যদিও এখনও অস্পষ্ট, কিছু বিশেষজ্ঞ পরামর্শ দেন যে অত্যধিক ক্যালসিয়াম, বিশেষ করে পরিপূরকগুলিতে, হৃদরোগের ঝুঁকি বাড়াতে পারে।
ন্যাশনাল অ্যাকাডেমি অফ সায়েন্সেস, ইঞ্জিনিয়ারিং এবং মেডিসিনের স্বাস্থ্য ও মেডিসিন বিভাগ সুপারিশ করে যে পরিপূরক এবং খাদ্যের সম্মিলিতভাবে মোট ক্যালসিয়াম গ্রহণ, 50 বছরের বেশি বয়সী ব্যক্তিদের জন্য দৈনিক 2,000 মিলিগ্রামের বেশি হওয়া উচিত নয়।
Vitamin D
Vitamin D improves the body’s ability to absorb calcium and improves bone health in other ways. People can get some of their vitamin D from sunlight, but this might not be a good source if you live in a high latitude, if you’re housebound, or if you regularly use sunscreen or avoid the sun because of the risk of skin cancer.
Dietary sources of vitamin D include cod liver oil, trout and salmon. Many types of milk and cereal have been fortified with vitamin D.
Most people need at least 600 international units (IU) of vitamin D a day. That recommendation increases to 800 IU a day after age 70.
People without other sources of vitamin D and especially with limited sun exposure might need a supplement. Most multivitamin products contain between 600 and 800 IU of vitamin D. Up to 4,000 IU of vitamin D a day is safe for most people.
ভিটামিন ডি শরীরের ক্যালসিয়াম শোষণের ক্ষমতাকে উন্নত করে এবং অন্যান্য উপায়ে হাড়ের স্বাস্থ্যের উন্নতি করে। লোকেরা সূর্যালোক থেকে তাদের ভিটামিন ডি পেতে পারে, তবে আপনি যদি উচ্চ অক্ষাংশে থাকেন, আপনি যদি ঘরবন্দী হন, বা আপনি যদি নিয়মিত সানস্ক্রিন ব্যবহার করেন বা ত্বকের ক্যান্সারের ঝুঁকির কারণে সূর্যকে এড়িয়ে চলুন তবে এটি একটি ভাল উত্স হতে পারে না। .
ভিটামিন ডি এর খাদ্যতালিকাগত উৎস কড লিভার অয়েল, ট্রাউট এবং স্যামন অন্তর্ভুক্ত। অনেক ধরনের দুধ এবং সিরিয়াল ভিটামিন ডি দিয়ে শক্তিশালী করা হয়েছে।
বেশিরভাগ মানুষের প্রতিদিন কমপক্ষে 600 আন্তর্জাতিক ইউনিট (IU) ভিটামিন ডি প্রয়োজন। এই সুপারিশটি 70 বছর বয়সের পর দিনে 800 আইইউতে বৃদ্ধি পায়।
যাদের ভিটামিন ডি-এর অন্যান্য উৎস নেই এবং বিশেষ করে সীমিত সূর্যের সংস্পর্শে তাদের সম্পূরক প্রয়োজন হতে পারে। বেশিরভাগ মাল্টিভিটামিন পণ্যে 600 থেকে 800 আইইউ ভিটামিন ডি থাকে। বেশিরভাগ মানুষের জন্য দিনে 4,000 আইইউ পর্যন্ত ভিটামিন ডি নিরাপদ।
Exercise
Exercise can help you build strong bones and slow bone loss. Exercise will benefit your bones no matter when you start, but you’ll gain the most benefits if you start exercising regularly when you’re young and continue to exercise throughout your life.
Combine strength training exercises with weight-bearing and balance exercises. Strength training helps strengthen muscles and bones in your arms and upper spine. Weight-bearing exercises — such as walking, jogging, running, stair climbing, skipping rope, skiing and impact-producing sports — affect mainly the bones in your legs, hips and lower spine. Balance exercises such as tai chi can reduce your risk of falling especially as you get older.
ব্যায়াম আপনাকে শক্তিশালী হাড় তৈরি করতে এবং হাড়ের ক্ষয় ধীর করতে সাহায্য করতে পারে। আপনি যখনই ব্যায়াম শুরু করেন না কেন ব্যায়াম আপনার হাড়ের উপকার করবে, কিন্তু আপনি সবচেয়ে বেশি সুবিধা পাবেন যদি আপনি অল্প বয়সে নিয়মিত ব্যায়াম শুরু করেন এবং সারা জীবন ব্যায়াম চালিয়ে যান।
ওজন বহন এবং ভারসাম্য ব্যায়ামের সাথে শক্তি প্রশিক্ষণ ব্যায়াম একত্রিত করুন। শক্তি প্রশিক্ষণ আপনার বাহু এবং উপরের মেরুদণ্ডের পেশী এবং হাড়কে শক্তিশালী করতে সহায়তা করে। ওজন বহন করার ব্যায়াম – যেমন হাঁটা, জগিং, দৌড়ানো, সিঁড়ি আরোহণ, দড়ি এড়িয়ে যাওয়া, স্কিইং এবং প্রভাব তৈরিকারী খেলাধুলা – প্রধানত আপনার পায়ের হাড়, নিতম্ব এবং মেরুদণ্ডের নীচের অংশকে প্রভাবিত করে। তাই চি এর মত ব্যালেন্স ব্যায়াম আপনার পতনের ঝুঁকি কমাতে পারে বিশেষ করে আপনার বয়স বাড়ার সাথে সাথে।
Diagnosis
Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of mineral in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only certain bones are checked — usually in the hip and spine.
আপনার হাড়ের ঘনত্ব একটি মেশিন দ্বারা পরিমাপ করা যেতে পারে যা আপনার হাড়ের খনিজ অনুপাত নির্ধারণ করতে কম মাত্রার এক্স-রে ব্যবহার করে। এই ব্যথাহীন পরীক্ষার সময়, একটি স্ক্যানার আপনার শরীরের উপর দিয়ে যাওয়ার সময় আপনি একটি প্যাডযুক্ত টেবিলে শুয়ে থাকেন। বেশিরভাগ ক্ষেত্রে, শুধুমাত্র নির্দিষ্ট হাড় পরীক্ষা করা হয় – সাধারণত নিতম্ব এবং মেরুদণ্ডে।
Treatment
Treatment recommendations are often based on an estimate of your risk of breaking a bone in the next 10 years using information such as the bone density test. If your risk isn’t high, treatment might not include medication and might focus instead on modifying risk factors for bone loss and falls.
চিকিত্সার সুপারিশগুলি প্রায়শই হাড়ের ঘনত্ব পরীক্ষার মতো তথ্য ব্যবহার করে পরবর্তী 10 বছরে আপনার হাড় ভাঙার ঝুঁকির অনুমানের উপর ভিত্তি করে। আপনার ঝুঁকি বেশি না হলে, চিকিৎসায় ওষুধ অন্তর্ভুক্ত নাও হতে পারে এবং এর পরিবর্তে হাড়ের ক্ষয় এবং পতনের ঝুঁকির কারণগুলি সংশোধন করার উপর ফোকাস করতে পারে।
Bisphosphonates
For both men and women at increased risk of broken bones, the most widely prescribed osteoporosis medications are bisphosphonates. Examples include:
- Alendronate (Binosto, Fosamax).
- Risedronate (Actonel, Atelvia).
- Ibandronate.
- Zoledronic acid (Reclast, Zometa).
ভাঙ্গা হাড়ের ঝুঁকিতে থাকা পুরুষ এবং মহিলা উভয়ের জন্য, অস্টিওপরোসিসের সবচেয়ে ব্যাপকভাবে নির্ধারিত ওষুধ হল বিসফসফোনেটস। উদাহরণ অন্তর্ভুক্ত:
- অ্যালেন্ড্রোনেট (বিনোস্টো, ফোসাম্যাক্স)।
- Risedronate (Actonel, Atelvia)।
- Ibandronate.
- জোলেড্রনিক অ্যাসিড (রিক্লাস্ট, জোমেটা)।
Side effects include nausea, abdominal pain and heartburn-like symptoms. These are less likely to occur if the medicine is taken properly. Intravenous forms of bisphosphonates don’t cause stomach upset but can cause fever, headache and muscle aches.
A very rare complication of bisphosphonates is a break or crack in the middle of the thighbone. A second rare complication is delayed healing of the jawbone, called osteonecrosis of the jaw. This can occur after an invasive dental procedure, such as removing a tooth.
পার্শ্ব প্রতিক্রিয়াগুলির মধ্যে রয়েছে বমি বমি ভাব, পেটে ব্যথা এবং অম্বল-সদৃশ লক্ষণ। সঠিকভাবে ওষুধ সেবন করলে এগুলি হওয়ার সম্ভাবনা কম থাকে। বিসফোসফোনেটের শিরায় পেট খারাপ হয় না তবে জ্বর, মাথাব্যথা এবং পেশীতে ব্যথা হতে পারে।
বিসফসফোনেটসের একটি খুব বিরল জটিলতা হল ঊরুর হাড়ের মাঝখানে একটি বিরতি বা ফাটল। দ্বিতীয় বিরল জটিলতা হল চোয়ালের হাড়ের নিরাময় বিলম্বিত, যাকে চোয়ালের অস্টিওনেক্রোসিস বলা হয়। এটি একটি আক্রমণাত্মক দাঁতের পদ্ধতির পরে ঘটতে পারে, যেমন একটি দাঁত অপসারণ।
Denosumab
Compared with bisphosphonates, denosumab (Prolia, Xgeva) produces similar or better bone density results and reduces the chance of all types of breaks. Denosumab is delivered via a shot under the skin every six months.
Similar to bisphosphonates, denosumab has the same rare complication of causing breaks or cracks in the middle of the thighbone and osteonecrosis of the jaw. If you take denosumab, you might need to continue to do so indefinitely. Recent research indicates there could be a high risk of spinal column fractures after stopping the drug.
বিসফোসফোনেটের সাথে তুলনা করে, ডেনোসুমাব (প্রোলিয়া, এক্সগেভা) হাড়ের ঘনত্বের অনুরূপ বা ভালো ফলাফল দেয় এবং সব ধরনের ভাঙার সম্ভাবনা কমায়। ডেনোসুমাব প্রতি ছয় মাসে ত্বকের নিচে একটি শটের মাধ্যমে বিতরণ করা হয়।
বিসফোসফোনেটের মতো, ডেনোসুমাবের ঊরুর হাড় এবং চোয়ালের অস্টিওনেক্রোসিসের মাঝখানে ভাঙ্গন বা ফাটল সৃষ্টি করার একই বিরল জটিলতা রয়েছে। আপনি যদি denosumab গ্রহণ করেন, তাহলে আপনাকে অনির্দিষ্টকালের জন্য এটি চালিয়ে যেতে হবে। সাম্প্রতিক গবেষণা ইঙ্গিত করে যে ওষুধ বন্ধ করার পরে মেরুদন্ডের কলাম ফাটলের উচ্চ ঝুঁকি থাকতে পারে।
Hormone-related therapy
Estrogen, especially when started soon after menopause, can help maintain bone density. However, estrogen therapy can increase the risk of breast cancer and blood clots, which can cause strokes. Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms also require treatment.
Raloxifene (Evista) mimics estrogen’s beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen. Taking this drug can reduce the risk of some types of breast cancer. Hot flashes are a possible side effect. Raloxifene also may increase your risk of blood clots.
In men, osteoporosis might be linked with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help improve symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and thus are recommended alone or in addition to testosterone.
ইস্ট্রোজেন, বিশেষ করে যখন মেনোপজের পরে শুরু হয়, হাড়ের ঘনত্ব বজায় রাখতে সাহায্য করতে পারে। যাইহোক, ইস্ট্রোজেন থেরাপি স্তন ক্যান্সার এবং রক্ত জমাট বাঁধার ঝুঁকি বাড়াতে পারে, যা স্ট্রোকের কারণ হতে পারে। তাই, ইস্ট্রোজেন সাধারণত অল্প বয়স্ক মহিলাদের হাড়ের স্বাস্থ্যের জন্য ব্যবহৃত হয় বা মহিলাদের মধ্যে যাদের মেনোপজের লক্ষণগুলির জন্যও চিকিত্সার প্রয়োজন হয়৷
Raloxifene (Evista) ইস্ট্রোজেনের সাথে সম্পর্কিত কিছু ঝুঁকি ছাড়াই, পোস্টমেনোপজাল মহিলাদের হাড়ের ঘনত্বের উপর ইস্ট্রোজেনের উপকারী প্রভাবের অনুকরণ করে। এই ওষুধ সেবন কিছু ধরনের স্তন ক্যান্সারের ঝুঁকি কমাতে পারে। হট ফ্ল্যাশ একটি সম্ভাব্য পার্শ্ব প্রতিক্রিয়া। রালোক্সিফেন আপনার রক্ত জমাট বাঁধার ঝুঁকি বাড়াতে পারে।
পুরুষদের মধ্যে, অস্টিওপরোসিস টেস্টোস্টেরনের মাত্রায় ধীরে ধীরে বয়স-সম্পর্কিত পতনের সাথে যুক্ত হতে পারে। টেস্টোস্টেরন প্রতিস্থাপন থেরাপি কম টেস্টোস্টেরনের লক্ষণগুলিকে উন্নত করতে সাহায্য করতে পারে, তবে অস্টিওপরোসিস ওষুধগুলি অস্টিওপরোসিসের চিকিত্সার জন্য পুরুষদের মধ্যে আরও ভালভাবে অধ্যয়ন করা হয়েছে এবং তাই একা বা টেস্টোস্টেরন ছাড়াও সুপারিশ করা হয়।
Bone-building medicines
If you have severe osteoporosis or if the more common treatments for osteoporosis don’t work well enough, your doctor might suggest trying:
- Teriparatide (Bonsity, Forteo). This powerful drug is similar to parathyroid hormone and stimulates new bone growth. It’s given by daily injection under the skin for up to two years.
- Abaloparatide (Tymlos) is another drug similar to parathyroid hormone. This drug can be taken for only two years.
- Romosozumab (Evenity). This is the newest bone-building medicine to treat osteoporosis. It is given as an injection every month at your doctor’s office and is limited to one year of treatment.
আপনার যদি গুরুতর অস্টিওপরোসিস থাকে বা যদি অস্টিওপরোসিসের জন্য আরও সাধারণ চিকিত্সা যথেষ্ট ভাল কাজ না করে, আপনার ডাক্তার চেষ্টা করার পরামর্শ দিতে পারেন:
- Teriparatide (Bonsity, Forteo). এই শক্তিশালী ওষুধটি প্যারাথাইরয়েড হরমোনের মতো এবং নতুন হাড়ের বৃদ্ধিকে উদ্দীপিত করে। এটি দুই বছর পর্যন্ত ত্বকের নিচে দৈনিক ইনজেকশন দিয়ে দেওয়া হয়।
- অ্যাবালোপ্যারাটাইড (টাইমলোস) প্যারাথাইরয়েড হরমোনের অনুরূপ আরেকটি ওষুধ। এই ওষুধটি মাত্র দুই বছরের জন্য নেওয়া যেতে পারে।
- Romosozumab (Evenity). অস্টিওপোরোসিসের চিকিৎসার জন্য এটি হাড়-গঠনের নতুন ওষুধ। এটি আপনার ডাক্তারের অফিসে প্রতি মাসে একটি ইনজেকশন হিসাবে দেওয়া হয় এবং এটি এক বছরের চিকিত্সার মধ্যে সীমাবদ্ধ।
After you stop taking any of these bone-building medications, you generally will need to take another osteoporosis drug to maintain the new bone growth.
আপনি এই হাড়-গঠনের ওষুধগুলির যে কোনও একটি গ্রহণ বন্ধ করার পরে, নতুন হাড়ের বৃদ্ধি বজায় রাখার জন্য আপনাকে সাধারণত অন্য অস্টিওপরোসিস ওষুধ গ্রহণ করতে হবে।
Lifestyle and home remedies
These suggestions might help reduce your risk of developing osteoporosis or breaking bones:
- Don’t smoke. Smoking increases rates of bone loss and the chance of fracture.
- Limit alcohol. Consuming more than two alcoholic drinks a day may decrease bone formation. Being under the influence of alcohol also can increase your risk of falling.
- Prevent falls. Wear low-heeled shoes with nonslip soles and check your house for electrical cords, area rugs, and slippery surfaces that might cause you to fall. Keep rooms brightly lit, install grab bars just inside and outside your shower door, and make sure you can get into and out of your bed easily.
জীবনধারা এবং ঘরোয়া প্রতিকার
এই পরামর্শগুলি আপনার অস্টিওপরোসিস বা হাড় ভাঙার ঝুঁকি কমাতে সাহায্য করতে পারে:
- ধূমপান করবেন না। ধূমপান হাড় ক্ষয়ের হার এবং ফ্র্যাকচারের সম্ভাবনা বাড়ায়।
- অ্যালকোহল সীমিত করুন। দিনে দুটির বেশি অ্যালকোহলযুক্ত পানীয় গ্রহণ করলে হাড়ের গঠন কমে যেতে পারে। অ্যালকোহলের প্রভাবের অধীনে থাকা আপনার পতনের ঝুঁকি বাড়িয়ে তুলতে পারে।
- পতন রোধ করুন। ননসলিপ সোল সহ কম হিলের জুতা পরুন এবং আপনার ঘরের বৈদ্যুতিক দড়ি, এলাকার রাগ এবং পিচ্ছিল পৃষ্ঠের জন্য পরীক্ষা করুন যা আপনার পড়ে যেতে পারে। ঘরগুলি উজ্জ্বলভাবে আলোকিত রাখুন, আপনার ঝরনার দরজার ঠিক ভিতরে এবং বাইরে গ্র্যাব বারগুলি ইনস্টল করুন এবং নিশ্চিত করুন যে আপনি সহজেই আপনার বিছানায় প্রবেশ করতে এবং বের হতে পারেন।
Arthritis
Osteoarthritis
The most common type of arthritis, osteoarthritis involves wear and tear damage to a joint’s cartilage — the hard, slick coating on the ends of bones where they form a joint. Cartilage cushions the ends of the bones and allows nearly frictionless joint motion, but enough damage can result in bone grinding directly on the bone, which causes pain and restricted movement. This wear and tear can occur over many years, or it can be hastened by a joint injury or infection.
Osteoarthritis also causes changes in the bones and deterioration of the connective tissues that attach muscle to bone and hold the joint together. If cartilage in a joint is severely damaged, the joint lining may become inflamed and swollen.
আর্থ্রাইটিস
অস্টিওআর্থারাইটিস
সবচেয়ে সাধারণ ধরনের আর্থ্রাইটিস, অস্টিওআর্থারাইটিসে জয়েন্টের তরুণাস্থির ক্ষতি হয় – হাড়ের প্রান্তে শক্ত, চটকদার আবরণ যেখানে তারা একটি জয়েন্ট তৈরি করে। তরুণাস্থি হাড়ের প্রান্তগুলিকে কুশন করে এবং প্রায় ঘর্ষণহীন জয়েন্ট গতির অনুমতি দেয়, কিন্তু যথেষ্ট ক্ষতির ফলে হাড় সরাসরি হাড়ের উপর নাকাল হতে পারে, যা ব্যথা এবং সীমিত নড়াচড়ার কারণ হয়। এই পরিধান এবং টিয়ার অনেক বছর ধরে ঘটতে পারে, অথবা এটি একটি যৌথ আঘাত বা সংক্রমণ দ্বারা ত্বরান্বিত হতে পারে।
অস্টিওআর্থারাইটিস হাড়ের পরিবর্তন এবং সংযোগকারী টিস্যুগুলির অবনতির কারণ হয় যা হাড়ের সাথে পেশী সংযুক্ত করে এবং জয়েন্টকে একত্রে ধরে রাখে। জয়েন্টের তরুণাস্থি মারাত্মকভাবে ক্ষতিগ্রস্ত হলে জয়েন্টের আস্তরণ স্ফীত এবং ফুলে যেতে পারে।
Rheumatoid arthritis
In rheumatoid arthritis, the body’s immune system attacks the lining of the joint capsule, a tough membrane that encloses all the joint parts. This lining (synovial membrane) becomes inflamed and swollen. The disease process can eventually destroy cartilage and bone within the joint.
রিউমাটয়েড আর্থ্রাইটিস
রিউমাটয়েড আর্থ্রাইটিসে, শরীরের ইমিউন সিস্টেম জয়েন্ট ক্যাপসুলের আস্তরণে আক্রমণ করে, একটি শক্ত ঝিল্লি যা সমস্ত জয়েন্ট অংশকে ঘিরে রাখে। এই আস্তরণ (সাইনোভিয়াল মেমব্রেন) স্ফীত এবং ফুলে যায়। রোগ প্রক্রিয়া অবশেষে জয়েন্টের মধ্যে তরুণাস্থি এবং হাড় ধ্বংস করতে পারে।
Risk factors
Risk factors for arthritis include:
- Family history. Some types of arthritis run in families, so you may be more likely to develop arthritis if your parents or siblings have the disorder.
- Age. The risk of many types of arthritis — including osteoarthritis, rheumatoid arthritis and gout — increases with age.
- Your sex. Women are more likely than men to develop rheumatoid arthritis, while most of the people who have gout, another type of arthritis, are men.
- Previous joint injury. People who have injured a joint, perhaps while playing a sport, are more likely to eventually develop arthritis in that joint.
- Obesity. Carrying excess pounds puts stress on joints, particularly your knees, hips and spine. People with obesity have a higher risk of developing arthritis.
ঝুঁকির কারণ
আর্থ্রাইটিসের ঝুঁকির কারণগুলির মধ্যে রয়েছে:
- পারিবারিক ইতিহাস। কিছু ধরণের আর্থ্রাইটিস পরিবারে চলে, তাই আপনার বাবা-মা বা ভাইবোনের ব্যাধি থাকলে আপনার বাত হওয়ার সম্ভাবনা বেশি হতে পারে।
- বয়স। অস্টিওআর্থারাইটিস, রিউমাটয়েড আর্থ্রাইটিস এবং গাউট সহ অনেক ধরণের বাতের ঝুঁকি বয়সের সাথে বৃদ্ধি পায়।
- তোমার সেক্স। পুরুষদের তুলনায় মহিলাদের রিউমাটয়েড আর্থ্রাইটিস হওয়ার সম্ভাবনা বেশি, যখন গাউট, অন্য ধরনের আর্থ্রাইটিস আছে তাদের অধিকাংশই পুরুষ।
- পূর্ববর্তী জয়েন্ট ইনজুরি। যে সমস্ত লোকেরা একটি জয়েন্টে আঘাত করেছে, সম্ভবত একটি খেলা খেলতে গিয়ে, শেষ পর্যন্ত সেই জয়েন্টে আর্থ্রাইটিস হওয়ার সম্ভাবনা বেশি।
- স্থূলতা। অতিরিক্ত পাউন্ড বহন করা জয়েন্টগুলিতে, বিশেষ করে আপনার হাঁটু, নিতম্ব এবং মেরুদণ্ডে চাপ দেয়। স্থূলতায় আক্রান্ত ব্যক্তিদের আর্থ্রাইটিস হওয়ার ঝুঁকি বেশি থাকে
Complications
Severe arthritis, particularly if it affects your hands or arms, can make it difficult for you to do daily tasks. Arthritis of weight-bearing joints can keep you from walking comfortably or sitting up straight. In some cases, joints may gradually lose their alignment and shape.
জটিলতা
গুরুতর আর্থ্রাইটিস, বিশেষ করে যদি এটি আপনার হাত বা বাহুকে প্রভাবিত করে, আপনার জন্য দৈনন্দিন কাজগুলি করা কঠিন করে তুলতে পারে। ওজন বহনকারী জয়েন্টের আর্থ্রাইটিস আপনাকে আরামে হাঁটা বা সোজা হয়ে বসতে বাধা দিতে পারে। কিছু ক্ষেত্রে, জয়েন্টগুলি ধীরে ধীরে তাদের প্রান্তিককরণ এবং আকৃতি হারাতে পারে।
Diagnosis
During the physical exam, doctors check your joints for swelling, redness, and warmth. They’ll also want to see how well you can move your joints.
রোগ নির্ণয়
শারীরিক পরীক্ষার সময়, ডাক্তাররা আপনার জয়েন্টগুলি ফুলে যাওয়া, লালভাব এবং উষ্ণতার জন্য পরীক্ষা করে। আপনি আপনার জয়েন্টগুলি কতটা ভালভাবে সরাতে পারেন তাও তারা দেখতে চাইবে।
Laboratory tests
The analysis of different types of body fluids can help pinpoint the type of arthritis you may have. Fluids commonly analyzed include blood, urine, and joint fluid. To obtain a sample of joint fluid, doctors cleanse and numb the area before inserting a needle in the joint space to withdraw some fluid.
ল্যাবরেটরি পরীক্ষা
বিভিন্ন ধরনের শরীরের তরল বিশ্লেষণ আপনার বাতের ধরন চিহ্নিত করতে সাহায্য করতে পারে। সাধারণত বিশ্লেষণ করা তরলগুলির মধ্যে রয়েছে রক্ত, প্রস্রাব এবং যৌথ তরল। জয়েন্ট ফ্লুইডের নমুনা পেতে, চিকিত্সকরা জয়েন্ট স্পেসে একটি সুই ঢোকানোর আগে কিছু তরল প্রত্যাহার করার জন্য জায়গাটি পরিষ্কার করে এবং অসাড় করে দেন।
Imaging
These types of tests can detect problems within the joint that may be causing your symptoms. Examples include:
- X-rays. Using low levels of radiation to visualize bone, X-rays can show cartilage loss, bone damage and bone spurs. Xrays may not reveal early arthritic damage, but they are often used to track progression of the disease.
- Computerized tomography (CT). CT scanners take X-rays from many different angles and combine the information to create cross-sectional views of internal structures. CTs can visualize both bone and the surrounding soft tissues.
- Magnetic resonance imaging (MRI). Combining radio waves with a strong magnetic field, MRIs can produce more-detailed cross-sectional images of soft tissues such as cartilage, tendons and ligaments.
- Ultrasound. This technology uses high-frequency sound waves to image soft tissues, cartilage and fluid-containing structures near the joints (bursae). Ultrasound is also used to guide needle placement for removing joint fluid or injecting medications into the joint.
ইমেজিং
এই ধরনের পরীক্ষাগুলি জয়েন্টের মধ্যে সমস্যাগুলি সনাক্ত করতে পারে যা আপনার লক্ষণগুলির কারণ হতে পারে। উদাহরণ অন্তর্ভুক্ত:
- X-rays. হাড়ের কল্পনা করার জন্য নিম্ন স্তরের বিকিরণ ব্যবহার করে, এক্স-রে তরুণাস্থি ক্ষয়, হাড়ের ক্ষতি এবং হাড়ের স্পার দেখাতে পারে। এক্স-রেগুলি প্রাথমিক আর্থ্রাইটিক ক্ষতি প্রকাশ নাও করতে পারে, তবে এগুলি প্রায়শই রোগের অগ্রগতি ট্র্যাক করতে ব্যবহৃত হয়।
- Computerized tomography (CT). সিটি স্ক্যানারগুলি বিভিন্ন কোণ থেকে এক্স-রে নেয় এবং অভ্যন্তরীণ কাঠামোর ক্রস-বিভাগীয় দৃশ্য তৈরি করতে তথ্য একত্রিত করে। সিটিগুলি হাড় এবং আশেপাশের নরম টিস্যু উভয়ই কল্পনা করতে পারে।
- Magnetic resonance imaging (MRI). একটি শক্তিশালী চৌম্বক ক্ষেত্রের সাথে রেডিও তরঙ্গের সংমিশ্রণে, এমআরআইগুলি তরুণাস্থি, টেন্ডন এবং লিগামেন্টের মতো নরম টিস্যুগুলির আরও বিস্তারিত ক্রস-বিভাগীয় চিত্র তৈরি করতে পারে।
- Ultrasound. এই প্রযুক্তি উচ্চ-ফ্রিকোয়েন্সি শব্দ তরঙ্গ ব্যবহার করে জয়েন্টগুলির কাছাকাছি নরম টিস্যু, তরুণাস্থি এবং তরল-ধারণকারী কাঠামো চিত্রিত করতে। আল্ট্রাসাউন্ড জয়েন্টের তরল অপসারণ বা জয়েন্টে ওষুধ ইনজেকশন দেওয়ার জন্য সুই বসানোর নির্দেশ দিতেও ব্যবহৃত হয়।
Treatment
Arthritis treatment focuses on relieving symptoms and improving joint function. You may need to try several different treatments, or combinations of treatments, before you determine what works best for you.
চিকিৎসা
আর্থ্রাইটিস চিকিত্সা লক্ষণগুলি উপশম এবং জয়েন্ট ফাংশন উন্নত করার উপর দৃষ্টি নিবদ্ধ করে। আপনার জন্য কোনটি সবচেয়ে ভালো কাজ করে তা নির্ধারণ করার আগে আপনাকে বিভিন্ন চিকিৎসা বা চিকিৎসার সংমিশ্রণ চেষ্টা করতে হতে পারে।
Medications
The medications used to treat arthritis vary depending on the type of arthritis. Commonly used arthritis medications include:
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Examples include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stronger NSAIDs can cause stomach irritation and may increase your risk of heart attack or stroke. NSAIDs are also available as creams or gels, which can be rubbed on joints.
- Counterirritants. Some varieties of creams and ointments contain menthol or capsaicin, the ingredient that makes hot peppers spicy. Rubbing these preparations on the skin over your aching joint may interfere with the transmission of pain signals from the joint itself.
- Steroids. Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage.
ওষুধ
আর্থ্রাইটিসের চিকিৎসার জন্য ব্যবহৃত ওষুধগুলি বাতের ধরনের উপর নির্ভর করে পরিবর্তিত হয়। সাধারণত ব্যবহৃত আর্থ্রাইটিস ওষুধের মধ্যে রয়েছে:
- NSAIDs: ননস্টেরয়েডাল অ্যান্টি-ইনফ্ল্যামেটরি ড্রাগস (NSAIDs) ব্যথা উপশম করতে পারে এবং প্রদাহ কমাতে পারে। উদাহরণগুলির মধ্যে রয়েছে ibuprofen (Advil, Motrin IB, অন্যান্য) এবং naproxen সোডিয়াম (Aleve)। শক্তিশালী NSAIDs পেটে জ্বালা সৃষ্টি করতে পারে এবং আপনার হার্ট অ্যাটাক বা স্ট্রোকের ঝুঁকি বাড়াতে পারে। এনএসএআইডিগুলি ক্রিম বা জেল হিসাবেও পাওয়া যায়, যা জয়েন্টগুলিতে ঘষে দেওয়া যেতে পারে।
- প্রতিরোধক। কিছু ধরণের ক্রিম এবং মলম মেন্থল বা ক্যাপসাইসিন ধারণ করে, যে উপাদানটি গরম মরিচকে মশলাদার করে তোলে। আপনার ব্যথাযুক্ত জয়েন্টের উপর ত্বকে এই প্রস্তুতিগুলি ঘষলে জয়েন্ট থেকেই ব্যথা সংকেত প্রেরণে হস্তক্ষেপ হতে পারে।
- স্টেরয়েড। কর্টিকোস্টেরয়েড ওষুধ, যেমন প্রিডনিসোন, প্রদাহ এবং ব্যথা এবং ধীর জয়েন্টের ক্ষতি কমায়।
Corticosteroids may be given as a pill or as an injection into the painful joint. Side effects may include thinning of bones, weight gain and diabetes.
- Disease-modifying antirheumatic drugs (DMARDs). These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. In addition to conventional DMARDs, there are also biologic agents and targeted synthetic DMARDs. Side effects vary but most DMARDs increase your risk of infections.
- Therapy Physical therapy can be helpful for some types of arthritis. Exercises can improve range of motion and strengthen the muscles surrounding joints. In some cases, splints or braces may be warranted.
কর্টিকোস্টেরয়েডগুলি একটি বড়ি হিসাবে বা বেদনাদায়ক জয়েন্টে ইনজেকশন হিসাবে দেওয়া যেতে পারে। পার্শ্ব প্রতিক্রিয়াগুলির মধ্যে হাড় পাতলা হওয়া, ওজন বৃদ্ধি এবং ডায়াবেটিস অন্তর্ভুক্ত থাকতে পারে।
- রোগ-সংশোধনকারী অ্যান্টি-রিউমেটিক ওষুধ (DMARDs)। এই ওষুধগুলি রিউমাটয়েড আর্থ্রাইটিসের অগ্রগতি মন্থর করতে পারে এবং জয়েন্টগুলি এবং অন্যান্য টিস্যুগুলিকে স্থায়ী ক্ষতি থেকে বাঁচাতে পারে। প্রচলিত DMARDs ছাড়াও, জৈবিক এজেন্ট এবং লক্ষ্যযুক্ত সিন্থেটিক DMARD আছে। পার্শ্ব প্রতিক্রিয়া পরিবর্তিত হয় তবে বেশিরভাগ DMARD আপনার সংক্রমণের ঝুঁকি বাড়ায়।
- থেরাপি শারীরিক থেরাপি কিছু ধরণের আর্থ্রাইটিসের জন্য সহায়ক হতে পারে। ব্যায়াম গতির পরিসর উন্নত করতে পারে এবং জয়েন্টগুলির পার্শ্ববর্তী পেশীগুলিকে শক্তিশালী করতে পারে। কিছু ক্ষেত্রে, স্প্লিন্ট বা ধনুর্বন্ধনী নিশ্চিত করা যেতে পারে।
Surgery
If conservative measures don’t help, doctors may suggest surgery, such as:
- Joint repair. In some instances, joint surfaces can be smoothed or realigned to reduce pain and improve function. These types of procedures can often be performed arthroscopically — through small incisions over the joint.
- Joint replacement. This procedure removes the damaged joint and replaces it with an artificial one. Joints most commonly replaced are hips and knees.
- Joint fusion. This procedure is more often used for smaller joints, such as those in the wrist, ankle and fingers. It removes the ends of the two bones in the joint and then locks those ends together until they heal into one rigid unit.
সার্জারি
যদি রক্ষণশীল ব্যবস্থাগুলি সাহায্য না করে, ডাক্তাররা অস্ত্রোপচারের পরামর্শ দিতে পারেন, যেমন:
যৌথ মেরামত। কিছু ক্ষেত্রে, ব্যথা কমাতে এবং কার্যকারিতা উন্নত করতে জয়েন্টের পৃষ্ঠতলগুলিকে মসৃণ বা পুনরায় সাজানো যেতে পারে। এই ধরনের পদ্ধতিগুলি প্রায়শই আর্থ্রোস্কোপিকভাবে সঞ্চালিত হতে পারে – জয়েন্টের উপর ছোট ছিদ্রের মাধ্যমে।
যৌথ প্রতিস্থাপন। এই পদ্ধতি ক্ষতিগ্রস্ত জয়েন্ট অপসারণ এবং একটি কৃত্রিম এক সঙ্গে এটি প্রতিস্থাপন। জয়েন্টগুলি সাধারণত প্রতিস্থাপিত হয় নিতম্ব এবং হাঁটু।
জয়েন্ট ফিউশন। এই পদ্ধতিটি প্রায়শই ছোট জয়েন্টগুলির জন্য ব্যবহৃত হয়, যেমন কব্জি, গোড়ালি এবং আঙ্গুলের মধ্যে। এটি জয়েন্টের দুটি হাড়ের প্রান্তগুলি সরিয়ে দেয় এবং তারপর সেই প্রান্তগুলিকে একত্রে লক করে যতক্ষণ না তারা একটি শক্ত ইউনিটে পরিণত হয়।
Lifestyle and home remedies
In many cases, arthritis symptoms can be reduced with the following measures:
- Weight loss. Excess weight puts extra stress on weightbearing joints. Losing weight may increase your mobility and limit future joint injury.
- Exercise. Regular exercise can help keep joints flexible. Swimming and water aerobics may be good choices because the buoyancy of the water reduces stress on weight-bearing joints.
- Heat and cold. Heating pads or ice packs may help relieve arthritis pain.
- Assistive devices. Using canes, shoe inserts, walkers, raised toilet seats, and other assistive devices can help protect joints and improve your ability to perform daily tasks.
জীবনধারা এবং ঘরোয়া প্রতিকার
অনেক ক্ষেত্রে, বাতের উপসর্গগুলি নিম্নলিখিত ব্যবস্থাগুলির মাধ্যমে হ্রাস করা যেতে পারে:
- ওজন হ্রাস। অতিরিক্ত ওজন ওজন বহনকারী জয়েন্টগুলিতে অতিরিক্ত চাপ দেয়। ওজন হ্রাস আপনার গতিশীলতা বাড়াতে পারে এবং ভবিষ্যতের জয়েন্টের আঘাতকে সীমিত করতে পারে।
- ব্যায়াম। নিয়মিত ব্যায়াম জয়েন্টগুলোকে নমনীয় রাখতে সাহায্য করতে পারে। সাঁতার এবং জলের অ্যারোবিকস ভাল পছন্দ হতে পারে কারণ জলের উচ্ছ্বাস ওজন বহনকারী জয়েন্টগুলিতে চাপ কমায়।
- তাপ এবং ঠান্ডা। হিটিং প্যাড বা আইস প্যাক বাতের ব্যথা উপশম করতে সাহায্য করতে পারে।
- সহায়ক ডিভাইস। বেত, জুতা সন্নিবেশ, ওয়াকার, উত্থাপিত টয়লেট সিট এবং অন্যান্য সহায়ক ডিভাইসগুলি জয়েন্টগুলিকে রক্ষা করতে এবং প্রতিদিনের কাজগুলি সম্পাদন করার ক্ষমতা উন্নত করতে সহায়তা করতে পারে।
Alternative medicine
Many people use alternative remedies for arthritis, but there is little reliable evidence to support the use of many of these products. The most promising alternative remedies for arthritis include:
- Acupuncture. This therapy uses fine needles inserted at specific points on the skin to reduce many types of pain, including that caused by some types of arthritis.
- Glucosamine. Although study results have been mixed, some studies have found that glucosamine works no better than placebo. However, glucosamine and the placebo both relieved osteoarthritis pain better than taking nothing, particularly in people who have moderate to severe pain from knee osteoarthritis.
- Chondroitin. Chondroitin may provide modest pain relief from osteoarthritis, although study results are mixed.
- Fish oil. Some preliminary studies have found that fish oil supplements may reduce the symptoms of some types of arthritis. Fish oil can interfere with medications, so check with your doctor first.
- Yoga and tai chi. The slow, stretching movements associated with yoga and tai chi may help improve joint flexibility and range of motion.
- Massage. Light stroking and kneading of muscles may increase blood flow and warm affected joints, temporarily relieving pain. Make sure your massage therapist knows which joints are affected by arthritis.
বিকল্প ঔষধ
অনেক লোক বাতের জন্য বিকল্প প্রতিকার ব্যবহার করে, তবে এই পণ্যগুলির অনেকগুলি ব্যবহারকে সমর্থন করার জন্য খুব কম নির্ভরযোগ্য প্রমাণ নেই। আর্থ্রাইটিসের জন্য সবচেয়ে প্রতিশ্রুতিবদ্ধ বিকল্প প্রতিকারগুলির মধ্যে রয়েছে:
- আকুপাংচার। এই থেরাপিটি ত্বকের নির্দিষ্ট বিন্দুতে ঢোকানো সূক্ষ্ম সূঁচ ব্যবহার করে অনেক ধরণের ব্যথা কমাতে, যার মধ্যে কিছু ধরণের আর্থ্রাইটিস হয়।
- গ্লুকোসামিন। যদিও অধ্যয়নের ফলাফলগুলি মিশ্রিত হয়েছে, কিছু গবেষণায় দেখা গেছে যে গ্লুকোসামিন প্লাসিবোর চেয়ে ভাল কাজ করে না। যাইহোক, গ্লুকোসামিন এবং প্লাসিবো উভয়ই অস্টিওআর্থারাইটিস ব্যথা থেকে মুক্তি দেয় কিছুই না খাওয়ার চেয়ে, বিশেষ করে যাদের হাঁটুর অস্টিওআর্থারাইটিস থেকে মাঝারি থেকে গুরুতর ব্যথা রয়েছে তাদের ক্ষেত্রে।
- কনড্রয়েটিন। চন্ড্রয়েটিন অস্টিওআর্থারাইটিস থেকে সামান্য ব্যথা উপশম প্রদান করতে পারে, যদিও অধ্যয়নের ফলাফল মিশ্রিত।
- মাছের তেল। কিছু প্রাথমিক গবেষণায় দেখা গেছে যে মাছের তেলের সম্পূরকগুলি কিছু ধরণের আর্থ্রাইটিসের লক্ষণগুলি কমাতে পারে। মাছের তেল ওষুধে হস্তক্ষেপ করতে পারে, তাই প্রথমে আপনার ডাক্তারের সাথে যোগাযোগ করুন।
- যোগব্যায়াম এবং তাই চি. যোগব্যায়াম এবং তাই চি এর সাথে যুক্ত ধীর, প্রসারিত নড়াচড়া যৌথ নমনীয়তা এবং গতির পরিসর উন্নত করতে সাহায্য করতে পারে।
- ম্যাসেজ। হাল্কা স্ট্রোক এবং পেশী গুলিয়ে রক্ত প্রবাহ বৃদ্ধি এবং প্রভাবিত জয়েন্টগুলি গরম হতে পারে, অস্থায়ীভাবে ব্যথা উপশম করতে পারে। নিশ্চিত করুন যে আপনার ম্যাসেজ থেরাপিস্ট জানেন যে কোন জয়েন্টগুলি বাতের দ্বারা প্রভাবিত হয়।
Gout
Gout is a painful form of arthritis. When your body has extra uric acid, sharp crystals can form in your joints (usually your big toe). Flare-ups of symptoms like pain and swelling come and go in periods called gout attacks. Treatment is usually a combination of symptom management and changing your diet.
গাউট
গাউট বাতের একটি বেদনাদায়ক রূপ। যখন আপনার শরীরে অতিরিক্ত ইউরিক অ্যাসিড থাকে, তখন আপনার জয়েন্টগুলোতে (সাধারণত আপনার বুড়ো আঙুল) ধারালো স্ফটিক তৈরি হতে পারে। পিরিয়ডের মধ্যে ব্যথা এবং ফুলে যাওয়ার মতো উপসর্গের ফ্লেয়ার-আপগুলিকে গাউট অ্যাটাক বলা হয়। চিকিত্সা সাধারণত লক্ষণ ব্যবস্থাপনা এবং আপনার খাদ্য পরিবর্তনের সমন্বয়।
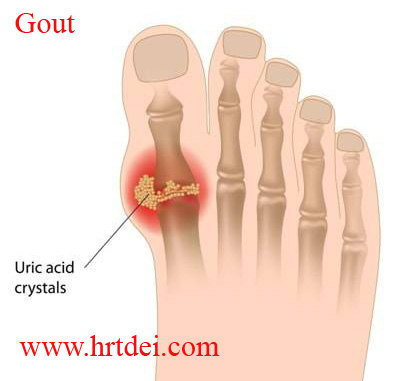
What is gout?
Gout is a form of inflammatory arthritis that causes pain and swelling in your joints. Gout happens when there’s a buildup of uric acid in your body.
গাউট কি?
গেঁটেবাত হল প্রদাহজনক আর্থ্রাইটিসের একটি রূপ যা আপনার জয়েন্টগুলোতে ব্যথা এবং ফোলাভাব সৃষ্টি করে। আপনার শরীরে ইউরিক অ্যাসিড জমা হলে গাউট হয়।
Gout most commonly affects your big toe joint. But it can affect other joints, including your:
গাউট সাধারণত আপনার বুড়ো আঙুলের জয়েন্টকে প্রভাবিত করে। কিন্তু এটি আপনার সহ অন্যান্য জয়েন্টগুলিকে প্রভাবিত করতে পারে:
- হাঁটু।
- গোড়ালি।
- পা।
- হাত ও কব্জি।
- কনুই।
Gout symptoms come and go (recur) in episodes called flares or gout attacks. A healthcare provider will suggest medications and changes to your diet that will lower your uric acid levels and minimize how often you experience gout attacks in the future.
গাউটের উপসর্গগুলি আসে এবং যায় (পুনরাবৃত্তি) পর্বে যাকে ফ্লেয়ার বা গাউট আক্রমণ বলা হয়। একজন স্বাস্থ্যসেবা প্রদানকারী ওষুধ এবং আপনার ডায়েটে পরিবর্তনের পরামর্শ দেবেন যা আপনার ইউরিক অ্যাসিডের মাত্রা কমিয়ে দেবে এবং ভবিষ্যতে আপনি কতবার গাউট আক্রমণের সম্মুখীন হবেন তা কমিয়ে দেবে।
Symptoms and Causes
What are gout symptoms?
Gout attacks are very painful and can happen suddenly, often overnight. During a gout attack, symptoms in your affected joints may include:
- Intense pain.
- Discoloration or redness.
- Stiffness.
- Swelling.,
- Tenderness, even to a light touch (like a bedsheet covering your affected joint).
- Warmth, or a feeling like the joint is “on fire.”
How long does a gout attack last?
Gout attacks usually last a week or two. You might have some flares that last longer than others, and some might cause more severe symptoms. Between attacks, you might not experience any gout symptoms.
What causes gout?
A buildup of excess uric acid in your body causes gout. Your body naturally makes uric acid when it breaks down chemicals called purines found in certain foods and drinks. Your kidneys usually filter uric acid out of your blood, and then it leaves your body when you pee. Sometimes your body makes too much uric acid, or your kidneys don’t remove it from your blood fast enough. When your body has high levels of uric acid (hyperuricemia), uric acid crystals can build up and settle into your joints. The sharp crystals clump together and cause sudden episodes of pain, swelling and other symptoms.Having temporarily high uric acid levels doesn’t mean you’ll definitely develop gout. Many people with hyperuricemia never get gout.
Gout risk factors
Gout can affect anyone. People assigned male at birth (AMAB) are three times more likely to develop gout. People assigned female at birth (AFAB) usually don’t experience gout until after menopause. People with certain health conditions are more likely to develop gout, including:
- Overweight or obesity.
- Congestive heart failure.
- Diabetes.
- Hypertension (high blood pressure).
- Kidney disease.
- Blood cancer.
You’re more likely to experience gout if you:
- Have a biological parent or grandparent who has gout.
- Eat a lot of animal proteins — especially animal flesh, shellfish and foods that contain organ meat.
- Drink alcohol regularly.
- Take a diuretic medication (water pills).
- Take immunosuppressants.
Which foods cause gout?
Eating or drinking foods high in purines are more likely to lead to high uric acid levels in your body that cause gout, including:
- Sugary drinks and sweets: Standard table sugar is half fructose (fruit sugar), which breaks down into uric acid. Any food or drink with high sugar content can trigger gout.
- High fructose corn syrup: This is a concentrated form of fructose. Packaged food products and processed snacks can contain lots of high fructose corn syrup.
- Alcohol: Even though not all alcoholic drinks are high in purines, alcohol prevents your kidneys from eliminating uric acid, pulling it back into your body, where it continues to accumulate.
- Organ meats: These include liver, tripe, sweetbreads, brains and kidneys.
- Game meats: Specialties such as goose, veal and venison all contain high levels of purines.
- Certain seafood: Herring, scallops, mussels, codfish, tuna, trout and haddock.
- Red meat: Beef, lamb, pork and bacon.
- Turkey: Especially processed deli turkey.
- Gravy and meat sauces.
Diagnosis of Gout
A healthcare provider will diagnose gout with a physical exam. They’ll ask you about your symptoms and examine your affected joints. Tell your provider when you first noticed symptoms like pain and swelling in your joint and how often the symptoms come and go.
What tests will be done to diagnose gout?
Your healthcare provider might use a few imaging tests to take pictures of your affected joints. These tests can also show if gout has caused any changes in your joints. You might need:
- X-rays.
- Ultrasound.
- Magnetic resonance imaging (MRI).
- A CT (computed tomography) scan — specifically a dual-energy CT scan.
Other common tests to diagnose gout include:
- Blood tests to measure the uric acid in your blood.
- Joint aspiration — using a needle to remove a sample of fluid from inside a joint.
Management and Treatment
How is gout treated?
Treating gout is usually a combination of managing your symptoms during a flare and reducing how often you consume high-purine foods and drinks.
Gout medication
Your healthcare provider might suggest medications to help manage your symptoms, including:
- NSAIDs: Over-the-counter (OTC) NSAIDs, like ibuprofen and naproxen, can reduce pain and swelling during a gout attack. Some people with kidney disease, stomach ulcers and other health problems shouldn’t take NSAIDs. Talk to your provider before taking NSAIDs.
- Colchicine: Colchicine is a prescription medication that can reduce inflammation and pain if you take it within 24 hours of a gout attack.
- Corticosteroids: Corticosteroids are prescription medications that reduce inflammation. Your provider might prescribe oral (by mouth) pills. They may also inject corticosteroids into your affected joints or into a muscle near your joint (intramuscularly).
Your provider might prescribe medications to help lower your uric acid levels. The most common medications that lower uric acid include:
- Allopurinol.
- Febuxostat.
- Pegloticase.
- Probenecid.
Low purine diet for gout
Your healthcare provider may suggest you follow a low-purine diet. A low-purine diet encourages you to consume fewer foods and drinks with high purine content. This will help reduce uric acid in your body. It also encourages you to eat some select foods that may reduce your uric acid levels.
Can gout be cured?
There’s no cure for gout. You’ll experience fewer attacks once you work with a healthcare provider to find treatments that manage your symptoms and lower your uric acid levels.
Prevention of Gout
The best way to prevent gout is to limit how often you consume high-purine foods and drinks. Make sure you drink plenty of water to help your kidneys function better and avoid dehydration.
Getting regular exercise can help reduce stress on your joints and reduce your risk for obesity and other health conditions that make you more likely to develop gout.
Outlook / Prognosis
What can I expect if I have gout?
If you have gout, you should expect to have flares of symptoms that come and go. Flares can happen more frequently if you don’t get gout diagnosed and treated by a healthcare provider.
Some people with gout experience more severe or more frequent attacks right after starting treatment as the uric acid in their body adjusts to new medications or changes in their diet.
What’s the outlook for people with gout?
Most people with gout eventually find a combination of treatments and lifestyle tweaks to manage their symptoms and reduce how often they experience gout attacks. Gout is treatable, People who have a blood uric level lower than 6 mg/dL are much less likely to experience gout attacks.
Untreated gout can lead to permanent joint damage. The buildup of uric acid in your joints and soft tissue is called tophus. Some people with gout can also develop other health problems, including:
- Severe arthritis and changes to the shape of your joint (joint deformity).
- Tophi (the plural form of tophus — a buildup of uric acid in the joints and soft tissue).
- Kidney stones.
- Heart disease.
Management of Gout
When we have a gout attack, we can manage symptoms by:
- Avoiding alcohol and sweet drinks.
- Drinking plenty of water.
- Elevating your affected joints above the level of your heart as often as you can.
- Icing your joints. Wrap an ice pack in a thin towel or put a cold compress on your joint for 15-20 minutes at a time a few times a day.
- Limiting stress on your joint by avoiding intense exercise or physical activities.
Frozen Shoulder
Frozen Shoulder
Frozen shoulder or adhesive capsulitis is a shoulder condition causing limited range of motion. This condition occurs when the tissues in the shoulder joint become thicker and tighter. The common signs and symptoms of frozen shoulder may include stiffness and pain in the shoulder joints which usually get worsened within one to three years. Treatment for the frozen shoulder may include physical therapy, medications, surgery and other procedures.
Symptoms
Signs and symptoms of a frozen shoulder are normally worsened and developed over time. They are divided into three stages including:
- Freezing stage
People with this stage of frozen shoulder usually have pain when moving the shoulder which limits the range of motion.
- Frozen stage
During this stage, the pain may be relieved but the shoulder becomes stiffer and more difficult to use.
- Thawing stage
The range of motion is more limited. Moving the shoulder is obviously more difficult for people with this final stage of a frozen shoulder.
Causes
A capsule of connecting tissue encases the shoulder joint. When these connecting tissues become thicker and tighter, the movement of the shoulder is restricted. The reason why the tissues get thicken and tighten is still unclear. However, systemic diseases and immobilizing the shoulder for a long period, such as in people after surgery or arm fracture tend to be involved in developing this condition.
Risk factors
Several factors might increase the risk of a frozen shoulder including:
- Age and gender
Women at the age of 40 and older tend to have more risk of frozen shoulder.
- Immobilized or less mobilized shoulder
The risk of a frozen shoulder is increased in people who have prolonged immobility or less mobility of the shoulder. The cause of immobility or less mobility of the shoulder may include a broken arm, recovery after surgery, injury, or stroke.
- Systemic diseases
Some systemic diseases may encourage the development of frozen shoulders. For example:
-
- Diabetes
- Hypothyroidism
- Hyperthyroidism
- Cardiovascular disease
- Parkinson’s disease
- Tuberculosis
Diagnosis
The doctor may conduct a physical exam to check for the pain and evaluate active and passive range of motion since either of them can be affected. A numbing medicine might be injected in some cases. Normally, a frozen shoulder can be diagnosed by the physical exam and reviewing of signs and symptoms. However, to seek for other problems, the doctor may require to use some image tests, such as X-rays or MRI.
Treatment
The aims of the treatment are to control the pain and improve a better range of motion. Medications, therapy, surgery, and some procedures are the common treatments of frozen shoulders.
- Medications
The doctor may prescribe several medications, such as pain relievers and anti-inflammatory drugs to relieve the pain and inflammation.
- Therapy
The doctor or a physical therapist may advise you on some range-of-motion exercises to promote the mobility of the shoulder.
- Surgical and other procedures
Other treatments for frozen shoulder may include:
-
- Steroid injection. To reduce pain and promote shoulder mobility
- Joint distension. To stretch the connecting tissues and to promote an easier movement
- Shoulder manipulation. To loosen the tightened tissue
- Surgery. The doctor may perform surgery to remove scar tissue and adhesions inside the shoulder joint in people who do not react to other treatments.
Muscle Atrophy
Muscle Atrophy
Muscle atrophy is the wasting or thinning of muscle mass. It can be caused by disuse of your muscles or neurogenic conditions. Symptoms include a decrease in muscle mass, one limb being smaller than the other, and numbness, weakness, and tingling in your limbs. Disuse atrophy can be reversed with exercise and a healthy diet.
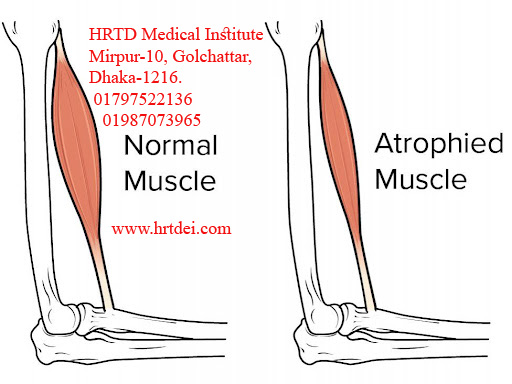
What is muscle atrophy?
Muscle atrophy is the loss or thinning of your muscle tissue. If you have atrophied muscles, you’ll see a decrease in your muscle mass and strength. With muscle atrophy, your muscles look smaller than normal. Muscle atrophy can occur due to malnutrition, age, genetics, a lack of physical activity, or certain medical conditions. Disuse (physiologic) atrophy occurs when you don’t use your muscles enough. Neurogenic atrophy occurs due to nerve problems or diseases.
Symptoms and Causes
What are the symptoms of muscle atrophy?
The symptoms of muscle atrophy differ depending on the cause of your condition. The most obvious sign of muscle atrophy is reduced muscle mass. Other signs of muscle atrophy may include:
- One arm or one leg is smaller than the other.
- Weakness in one arm and or one leg.
- Numbness or tingling in your arms and legs.
- Trouble walking or balancing.
- Difficulty swallowing or speaking.
- Facial weakness.
- Gradual memory loss.
What does muscle atrophy feel like?
If you have muscle atrophy in your limbs, you may feel tingling, numbness or weakness in your arms and legs. If you have atrophied muscles in your face or throat, your facial muscles may start feeling weak and you may find it difficult to speak or swallow.
What causes muscle atrophy?
The cause of muscle atrophy depends on the type you have. Disuse (physiologic) atrophy is caused by not using your muscles enough. If you stop using your muscles, your body won’t waste the energy it needs to take care of them. Instead, your body will start to break your muscles down, which causes them to decrease in size and strength. Disuse atrophy may affect you if you:
- Lead a sedentary lifestyle.
- Are malnourished.
- Don’t get enough exercise.
- Sit at a desk job all day.
- Are on best rest.
- Have a genetic disorder such as muscular dystrophy or Charcot-Marie-Tooth disease.
- Can’t move your limbs due to a stroke or other conditions such as dermatomyositis.
- Have age-related atrophy (sarcopenia).
Neurogenic atrophy is caused by an injury or disease affecting nerves that connect to your muscles. When these nerves are damaged, they can’t trigger the muscle contractions that are needed to stimulate muscle activity. When your muscles don’t contract, your body thinks you don’t need them anymore. So your body starts breaking them down, which causes them to decrease in size and strength. Diseases and other conditions that can affect these nerves include:
- Amyotrophic lateral sclerosis (ALS).
- Guillain-Barre syndrome.
- Carpal tunnel syndrome.
- Polio.
- Spinal cord injury.
- Multiple sclerosis.
How long does it take muscles to atrophy?
The amount of time it takes for your muscles to atrophy depends on your age, fitness level and cause of atrophy. If your muscle atrophy is due to disuse (physiologic), the process can start within two to three weeks of not using your muscles. Neurogenic muscle atrophy may develop sooner depending on your health condition.
Diagnosis and Tests
How is muscle atrophy diagnosed?
To diagnose muscle atrophy, your healthcare provider will give you a physical exam and ask you about your symptoms. They’ll look at your arms and legs and measure your muscle mass. In addition, your healthcare provider may order tests, including:
- Blood test.
- Muscle or nerve biopsy.
- Electromyography (EMG).
- Nerve conduction studies.
- X-rays.
- Computed tomography (CT) scan.
- Magnetic resonance imaging (MRI) scan.
Management and Treatment
Disuse (physiologic) atrophy can sometimes be reversed with exercise and a healthy diet. Your healthcare provider may start you on a program that includes exercises in the pool. Working out in the water can reduce your muscle workload. Neurogenic atrophy typically can’t be reversed because of the physical damage that’s been done to your nerves.
Treatment for muscle atrophy depends on the type. Disuse (physiologic) atrophy can be treated with regular exercise and better nutrition. Your healthcare provider may recommend physical therapy or an exercise plan. Even if you can’t actively move certain joints in your body, you can do still exercises wearing a splint or brace. Your healthcare provider may have you work with a dietitian on a healthy eating plan. They may suggest nutritional supplements as well.
Neurogenic atrophy can sometimes be treated with a special kind of physical therapy called electrical stimulation. Your physical therapist will place electrodes on your skin over your muscles. The electrodes send small electrical impulses to your nerves and muscles. The electrical impulses try to artificially exercise or contract your muscles. This can help you maintain your muscle mass and strength.
Your physical therapist may also recommend ultrasound therapy. Ultrasound therapy uses sound waves to promote muscle healing.
If you develop a contracture due to your muscle atrophy, your healthcare provider may perform surgery to correct it. A contracture occurs when your muscle tissues become fibrous. This tissue makes it hard for you to stretch the muscle and prevents movement.
Bone Fracture
A broken bone or bone fracture occurs when a force exerted against a bone is stronger than the bone can bear. This disturbs the structure and strength of the bone, and leads to pain, loss of function and sometimes bleeding and injury around the site.
There are different types of bone fractures. Some are more severe than others, depending on the strength and direction of the force, the particular bone involved, and the person’s age and general health. Common bone fractures include:
- wrist
- ankle
- hip – hip fractures occur most often in older people.
Broken bones take around 4 to 8 weeks to heal, depending on the age and health of the person and the type of break.
Causes of bone fractures
Causes of bone fractures can include:
- traumatic incidents such as sporting injuries, vehicle accidents and falls
- conditions such as osteoporosis and some types of cancer that cause bones to fracture more easily, meaning even minor trauma and falls can become serious.
Symptoms of bone fractures
Fractures are different from other injuries to the skeleton such as dislocations, although in some cases it can be hard to tell them apart. Sometimes, a person may have more than one type of injury. If in doubt, treat the injury as if it is a fracture.
The symptoms of a fracture depend on the particular bone and the severity of the injury, but may include:
- pain
- swelling
- bruising
- deformity
- inability to use the limb.
Types of bone fracture
Different types of fracture include:
- Closed (simple) fracture – the broken bone has not pierced the skin.
- Open (compound) fracture – the broken bone juts out through the skin, or a wound leads to the fracture site. Infection and external bleeding are more likely.
- Greenstick fracture – a small, slender crack in the bone. This can occur in children, because their bones are more flexible that an adult’s bones.
- Hairline fracture – the most common form is a stress fracture, often occurring in the foot or lower leg as a result of repeated stress from activities such as jogging or running.
- Complicated fracture – structures surrounding the fracture are injured. There may be damage to the veins, arteries or nerves, and there may also be injury to the lining of the bone (the periosteum).
- Comminuted fracture – the bone is shattered into small pieces. This type of complicated fracture tends to heal more slowly.
- Avulsion fracture – muscles are anchored to bone with tendons, a type of connective tissue. Powerful muscle contractions can wrench the tendon free and pull out pieces of bone. This type of fracture is more common in the knee and shoulder joints.
- Compression fracture – occurs when 2 bones are forced against each other. The bones of the spine, called vertebrae, can have this type of fracture. Older people, particularly those with osteoporosis, are at higher risk.
Not all fractures are of a person’s arm or leg. Trauma to the head, chest, spine or pelvis can fracture bones such as the skull and ribs. These fractures are further complicated by the underlying body structure that the bone normally protects.
Some of these fractures can be very difficult to manage using first-aid principles only, as they may represent life-threatening injuries. Always seek emergency assistance if you suspect this type of fracture.
Complications of bone fractures
Other problems caused by bone fracture can include:
- Blood loss – bones have a rich blood supply. A bad break can make you lose a large amount of blood.
- Injuries to organs, tissues or surrounding structures – for example the brain can be damaged by a skull fracture. Chest organs can be injured if a rib breaks.
- Stunted growth of the bone – if a child’s long bone breaks close to the joint where the growth plates are found.
First aid for bone fractures
Good first-aid care of fractures is important. Moving the broken bones can increase pain and bleeding and can damage tissues around the injury. This can lead to complications in the repair and healing of the injury later on.
First aid for fractures is all about immobilising (limiting movement of) the injured area. Splints can be used for this. Control any external bleeding.
Complicated breaks where a limb is very deformed may need to be realigned before splinting – only paramedics or medical staff should do this.
Fractures of the head or body such as skull, ribs and pelvis are all serious and should be managed by paramedics.
If you suspect a bone fracture, you should:
- Keep the person still – do not move them unless there is an immediate danger, especially if you suspect fracture of the skull, spine, ribs, pelvis or upper leg.
- Attend to any bleeding wounds first. Stop the bleeding by pressing firmly on the site with a clean dressing. If a bone is protruding, apply pressure around the edges of the wound.
- If bleeding is controlled, keep the wound covered with a clean dressing.
- Never try to straighten broken bones.
- For a limb fracture, provide support and comfort such as a pillow under the lower leg or forearm. However, do not cause further pain or unnecessary movement of the broken bone.
- Apply a splint to support the limb. Splints do not have to be professionally manufactured. Items like wooden boards and folded magazines can work for some fractures. You should immobilise the limb above and below the fracture.
- Use a sling to support an arm or collarbone fracture.
- Raise the fractured area if possible and apply a cold pack to reduce swelling and pain.
- Stop the person from eating or drinking anything until they are seen by a health care professional in case they need surgery.
- In an emergency, call triple zero (000) for an ambulance.
Diagnosis of bone fractures
Doctors can diagnose bone fractures with x-rays. They may also use CT scan (computed tomography) and MRI scans (magnetic resonance imaging).
Treatment of bone fractures
Broken bones heal by themselves – the aim of medical treatment is to make sure the pieces of bone are lined up correctly. The bone needs to recover fully in strength, movement and sensitivity. Some complicated fractures may need surgery or surgical traction (or both).
Depending on where the fracture is and how severe, treatment may include:
- splints – to stop movement of the broken limb
- braces – to support the bone
- plaster cast – to provide support and immobilise the bone
- traction – a less common option
- surgically inserted metal rods or plates – to hold the bone pieces together
- pain relief – to reduce pain.
Operation procedure for bone fractures
A cast made from plaster of Paris is one of the most common ways of immobilizing a limb. This cast is made from a preparation of gypsum that sets hard when water is added. Depending on the location and severity of the fracture, the operation procedures can include:
- Closed or simple fractures – the 2 ends of the broken bone are lined up and held in place. The limb is thoroughly bandaged, and then the wet plaster is applied. Sometimes, once the plaster is dry, the cast is split into 2 and the 2 halves are re-bandaged on the outside. This allows for any swelling that may occur.
- Open or compound fractures – these are thoroughly cleaned in the operating room to remove debris before being set, because a broken bone exposed to the open air may become infected.
- Long bones – Long bones such as the bone of the thigh (femur) are difficult to keep aligned. In adults, these are often treated by internal nailing. A child may need traction for a couple of days before setting the bone in a cast. Once the 2 ends of the bone start to show signs of healing, the leg and hip joint are immobilized in plaster of Paris. In other cases, pins are inserted above and below the fracture and secured to an external frame or ‘fixator’. This is done under a general anesthetic.
Immediately after an operation on a bone fracture
After surgery, your doctor will check that you have full feeling in the area. For example, if you have a broken arm in plaster, they may ask you to wiggle your fingers. They will also check your limb for tingling, pallor (pale color), or coolness. These tests check whether the splint is affecting your limb’s nerve and blood supply. The injured part is kept as still as possible in the first few days.
Nurses will offer you pain-relieving medication. They will determine the difference between the pain of your fracture and any pain that could be caused by the splint, traction, plaster cast, poor alignment of the limb or swelling of the limb.
The healing process for bone fractures
Blood clots that form on the broken ends of bone are the start of the healing process. Over about 5 weeks, the body joins the 2 bone portions together with a combination of fibrous cells and cartilage.
This temporary bone (callus) is not as strong as real bone. It can break easily until it is slowly replaced with real bone. For this reason the doctor may remove your cast or splint after a few weeks, but you still need to treat the bone with care for at least one more month.
Other treatments for bone fractures
Some bones, such as the collarbone or bones of the toes, are immobilized with a sling or splint (instead of plastered) and rested for about 2 months.
Complications of bone fractures
Possible complications of a bone fracture may include:
wrongly fitted plaster cast (for example, too tight or too loose).
poor alignment of the limb
infection
Muscle Cramp
A muscle cramp is an uncontrollable and painful spasm of a muscle. Any muscle can be affected, but the muscles of the calf and foot are particularly prone. A cramp can last for varying periods of time and generally resolves by itself. The exact cause of cramps is unknown but risk factors may include poor physical condition, mineral and electrolyte imbalances, and tight, inflexible muscles.
Cramps are usually harmless but may sometimes be symptomatic of an underlying medical disorder, such as atherosclerosis (narrowing of the arteries). Regular cramping or severe cramping that lasts longer than a few minutes should always be investigated by your doctor.
Symptoms of muscle cramps
The symptoms of a muscle cramp include:
- sudden sensation of uncontrollable and painful spasms in the muscle
- muscle twitching.
Minerals and electrolytes
Muscle tissue relies, in part, on a range of minerals, electrolytes, and other chemicals in order to contract and relax. Some of these important substances include calcium, magnesium, potassium, and sodium. Inadequate diet, dehydration, vomiting and diarrhoea are just some of the factors that are thought to disturb the body’s balance of minerals and electrolytes, and make muscles more susceptible to cramping.
Tetany is a special form of cramping – it can be brought on by overbreathing, which results in a low level of carbon dioxide in the blood. It is usually caused by anxiety.
Risk factors for muscle cramps
The exact cause of muscle cramp is not known, but risk factors may include:
- tight, inflexible muscles
- poor physical condition
- poor muscle tone
- inadequate diet
- physical overexertion
- physical exertion of cold muscles
- muscle injury
- muscle fatigue
- excessive perspiration
- dehydration – caused by, for example, a bout of gastroenteritis
- reduced blood supply (ischaemia)
- wearing high-heeled shoes for lengthy periods.
Muscle cramps associated with medical conditions
Certain diseases or conditions may increase the risk of muscle cramp, including:
- Atherosclerosis – a condition characterised by narrowed arteries due to the formation of fatty plaques. Muscles are more likely to cramp if their blood supply is inadequate.
- Sciatica – pain in the buttock and leg caused by pressure on nerves in the lower back. In some cases, the irritated nerve may prompt the associated muscles to contract.
- Medications – some medical conditions require the regular use of fluid pills (diuretics). These drugs can interfere with the body’s mineral balance and contribute to cramping.
Treatment options for muscle cramps
Most muscle cramps resolve after a few seconds or minutes. There has been very little research done to work out which treatment works best, but treatment options include:
- Stretch and massage – lengthen the cramping muscle using a gentle, sustained stretch then lightly massage the area until the cramp subsides. If you are unsure how to stretch leg muscles, see your physiotherapist for advice.
- Ice pack – in cases of severe cramps, an ice pack applied for a few minutes may help the muscle to relax.
- Medication – some medications can be helpful to control muscle cramps. See your doctor for further information.
- Further treatment – see your doctor if you experience regular muscle cramping or if cramps last longer than a few minutes. You may have an undiagnosed medical condition that requires treatment.
Prevention strategies
Suggestions on how to reduce the likelihood of muscle cramp include:
- Increase your level of physical fitness.
- Incorporate regular stretching into your fitness routine.
- Warm up and cool down thoroughly whenever you exercise or play sport.
- Drink plenty of water before, during and after exercise.
- Make sure your diet is nutritionally adequate, and include plenty of fruits and vegetables.
- A regular massage may help to reduce muscle tension.
- Wear properly fitted shoes and avoid high heels.
Fibromyalgia
Fibromyalgia causes pain in your muscles and joints throughout your body. It can also make you feel fatigued and cause mental symptoms like memory problems. Experts don’t know what causes fibromyalgia — and there’s no cure for it — but a healthcare provider will help you find treatments to manage your symptoms.
Fibromyalgia is a long-term (chronic) health condition that causes pain and tenderness throughout your body. It causes musculoskeletal pain and fatigue.
People with fibromyalgia usually experience symptoms that come and go in periods called flare-ups. Sometimes, it can feel exhausting and challenging to navigate living with fibromyalgia. The peaks and valleys between feeling good and suddenly having a flare-up of symptoms can feel overwhelming. Fibromyalgia is real, and so is how you feel.
Experts don’t know what causes fibromyalgia, but studies have found that certain health conditions, stress and other changes in your life might trigger it. You might be more likely to develop fibromyalgia if one of your biological parents has it.
Any new pain in your body is often the first sign of fibromyalgia — especially in your muscles. Trust your instincts and listen to your body. Visit a healthcare provider if you’re experiencing new pain, fatigue, and other symptoms — even if it feels like they come and go.
Who is affected by fibromyalgia?
Anyone can develop fibromyalgia. It affects people of any age, including children. Around 4 million people in the U.S. are living with fibromyalgia.
People assigned female at birth (AFAB) and people older than 40 are more likely to be diagnosed with fibromyalgia.
Symptoms and Causes
What are fibromyalgia symptoms?
The two most common symptoms of fibromyalgia are pain and fatigue. You may experience:
- Muscle pain or tenderness.
- Fatigue.
- Face and jaw pain (temporomandibular joint disorders).
- Headaches and migraines.
- Digestive problems, including diarrhea and constipation.
- Bladder control issues.
Fibromyalgia can cause mental and emotional symptoms, including:
- Memory problems (sometimes called “fibro fog” or “brain fog”).
- Anxiety.
- Depression.
- Insomnia and other sleep disorders.
What causes fibromyalgia?
Experts don’t know what causes fibromyalgia.
Certain genes you inherit from your biological parents might make you more likely to develop fibromyalgia. Studies have found a link between biological parents who have fibromyalgia and their children — this might mean it’s passed down through families.
People with fibromyalgia are usually more sensitive to pain than most people. Experts haven’t found the direct link yet, but they think genetic mutations in the genes responsible for forming the neurotransmitters in your brain that broadcast and receive pain signals to your body might cause fibromyalgia.
What are the risk factors for fibromyalgia?
Even though experts can’t say for sure what causes fibromyalgia, some health conditions and other issues are risk factors for developing it. Fibromyalgia risk factors include:
- Your age: People older than 40 are more likely to develop fibromyalgia. But it can affect anyone, including children.
- Your sex assigned at birth: People assigned female at birth are twice as likely to experience fibromyalgia.
- Chronic illnesses: People with conditions like osteoarthritis, depression, anxiety disorders, chronic back pain, and irritable bowel syndrome are more likely to develop fibromyalgia.
- Infections: Some people develop fibromyalgia after having an infection, especially if they experience severe symptoms.
- Stress: The amount of stress you experience can’t be measured on a test, but too much stress can affect your health.
- Traumas: People who’ve experienced a physical or emotional trauma or a serious injury sometimes develop fibromyalgia.
What triggers a fibromyalgia flare-up?
Certain events or changes in your life can trigger a fibromyalgia flare-up. Everyone is different, and what triggers symptoms for some people might not for you. In general, anything that increases your stress can trigger a flare-up, including:
- Emotional stress caused by your job, financial situation or social life.
- Changes in your daily routine.
- Changes in your diet or not getting enough nutrition.
- Hormone changes.
- Not getting enough sleep or changing when you sleep.
- Weather or temperature changes.
- Getting sick.
- Starting new medication or treatments, or changing something in your usual fibromyalgia treatment routine.
Diagnosis of Fibromyalgia
A healthcare provider will diagnose fibromyalgia with a physical exam and discussion of your health history. They’ll ask about your symptoms and when you first noticed them.
There’s no test that can diagnose fibromyalgia. Usually, diagnosing it is part of a differential diagnosis — a medical process of elimination. Your provider will make a diagnosis by comparing several conditions with related symptoms. This process leads to your final diagnosis.
Your provider might use blood tests to rule out other common causes of fatigue like anemia or issues with your thyroid gland.
Management and Treatment
There isn’t a single treatment that works for every person with fibromyalgia. Your provider will work with you to find a combination of treatments that relieve your symptoms. Tell your provider which symptoms you’re experiencing and when they change (including when they’re improving or getting worse).
Treatments you might need include:
- Over-the-counter (OTC) or prescription medicine to relieve pain.
- Exercises like stretches or strength training.
- Sleep therapy.
- Cognitive behavioral therapy.
- Stress management therapy.
- Antidepressants.
Four stages of fibromyalgia
Fibromyalgia is a dynamic condition. This means you won’t experience symptoms in any specific order — there’s no roadmap to know when or how fibromyalgia symptoms will affect you.
Your provider might treat your fibromyalgia in stages based on how you feel. These stages aren’t a step-by-step treatment plan. Every person is different, and how fibromyalgia affects your body will be unique. The stages are more like loose categories that can help you understand which treatments you’ll need to manage your symptoms. The four stages of treating fibromyalgia include:
- Non-pharmacological treatments: Your provider or a physical therapist will give you stretches and exercises to loosen, relax and strengthen your muscles and joints.
- Psychological treatments: A mental health professional will help you identify ways to maintain a healthy self-image. They’ll suggest strategies to manage symptoms that affect your mental and emotional health.
- Pharmacological treatment: Taking medicine to manage your symptoms.
- Daily functioning: An occupational therapist can help you navigate your daily routine if you’re experiencing severe symptoms that make it hard to participate in your regular activities.
Prevention of Fibromyalgia
Because experts don’t know what causes fibromyalgia, you can’t prevent it.
Maintaining your overall health can help reduce the severity of fibromyalgia symptoms:
- Manage stress as well as you can.
- Follow a diet and exercise plan that’s healthy for you.
- Get enough sleep and practice good sleep hygiene.
Outlook / Prognosis
What can I expect if I have fibromyalgia?
You should expect to manage fibromyalgia symptoms for a long time — maybe for the rest of your life. Some people with fibromyalgia experience fewer flare-ups with milder symptoms after they find treatments that work for them. Ask your provider how often you need follow-up appointments to adjust your treatments or to adjust any medications you’re taking.
Complications of fibromyalgia
People with fibromyalgia are more likely to be hospitalized because of pain, fatigue or mental health symptoms. You’re also more likely to experience memory problems and have trouble concentrating.
Talk to your provider as soon as you notice any changes in your symptoms, especially if you feel like they’re affecting your memory or mental health.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is when the median nerve is compressed as it passes through the carpal tunnel. The carpal tunnel is an opening in your wrist that is formed by the carpal bones on the bottom of the wrist and the transverse carpal ligament across the top of the wrist. The median nerve provides sensory and motor functions to the thumb and 3 middle fingers. If it gets compressed or irritated, you may have symptoms.
What You Need to Know
- Carpal tunnel release is one of the most common hand conditions requiring surgery.
- Symptoms may include tingling, pain, numbness or weakness in the thumb through ring fingers of the affected hand.
- Women get carpal tunnel syndrome three times more often than men.
- Carpal tunnel syndrome is a progressive condition that can worsen without proper care.
- Symptoms of carpal tunnel syndrome often occur during pregnancy and can be alleviated with nonsurgical treatments. Symptoms often improve after delivery, but such patients are at higher risk of developing carpal tunnel syndrome later in life.
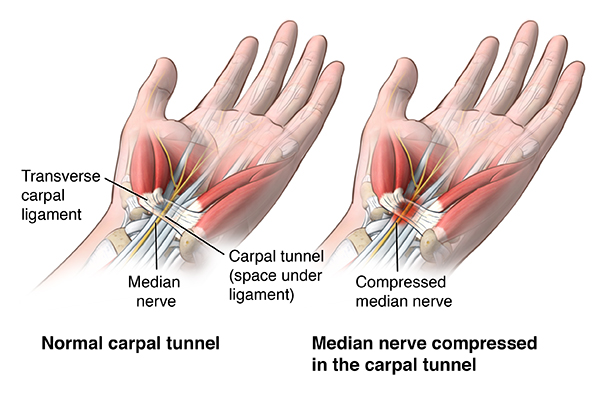
Carpal Tunnel Syndrome Causes and Risk Factors
Carpal tunnel syndrome is caused by an increase in pressure within the carpal tunnel, which leads to compression of the median nerve as it travels across the wrist into the palm through the carpal tunnel.
In most cases, this increase in pressure inside the carpal tunnel is difficult to attribute to one cause. Typically, multiple factors are at play that result in the pressure on the nerve:
- Anatomical changes and differences: The carpal tunnel opening is too narrow
- Some people may have smaller than average carpal tunnel size, which could run in families
- Women, on average, have smaller carpal tunnel size than men and are more likely to develop carpal tunnel syndrome
- Bones and joints could change shape over time due to diseases such as osteoarthritis or trauma to the wrist
- Swelling and inflammation: When tissues in and around the carpal tunnel swell up, they can press on the median nerve. Swelling and inflammation could result from:
- Frequent, repetitive movements with the hands
- Extending or flexing the wrist for long periods of time
- Rheumatoid arthritis and other conditions that cause inflammation in the joints
- Hormonal or metabolic changes (for example, menopause, pregnancy or thyroid imbalance)
- Other contributing factors:
- Changes in blood sugar levels (may be seen with type 2 diabetes)
- Other conditions or injuries of the wrist (for example, strain, sprain, dislocation or break)
- Obesity
What are the symptoms of carpal tunnel syndrome?
These are the most common symptoms:
- Weakness when gripping objects with one or both hands
- Pain or numbness in one or both hands
- “Pins and needles” feeling in the fingers
- Swollen feeling in the fingers
- Burning or tingling in the fingers, especially the thumb and the index and middle fingers
- Pain or numbness that is worse at night, interrupting sleep
The symptoms of carpal tunnel syndrome may be similar to other medical conditions or problems. Always see your healthcare provider for a diagnosis.
How is carpal tunnel syndrome diagnosed?
Your provider will check your medical history and give you a physical exam. He or she may recommend that you have electrodiagnostic tests on your nerves. These tests are the best way to diagnose carpal tunnel syndrome. Electrodiagnostic tests stimulate the muscles and nerves in your hand to see how well they work.
Treatment of carpal tunnel syndrome
Your healthcare provider will figure out the best treatment for you based on:
- Your age
- Your overall health and medical history
- How bad your wrist is right now
- How well do you tolerate specific medications, procedures, or therapies
- How bad the disease is expected to get
- Your opinion or preference
Treatment may include:
- Splinting your hand. This helps keep your wrist from moving. It also eases the compression of the nerves inside the tunnel.
- Anti-inflammatory medication. These may be oral or injected into the carpal tunnel space. These reduce the swelling.
- Surgery. This eases compression on the nerves in the carpal tunnel.
- Worksite changes. Changing position of your computer keyboard or making other ergonomic changes can help ease symptoms.
- Exercise. Stretching and strengthening exercises can be helpful in people whose symptoms have gotten better. These exercises may be supervised by a physical or occupational therapist.
Surgery for carpal tunnel syndrome
Surgery for carpal tunnel syndrome is usually done as an outpatient. Two types of carpal tunnel surgery are done: open surgery and endoscopic surgery. You may have local or general anesthesia, or both, for either surgery.
During open surgery, the surgeon cuts open your wrist. The tissue that is pressing on the nerves is cut. This relieves the pressure on the nerve.
During endoscopic surgery, the surgeon puts a long, thin rod through a tiny cut on the wrist. The rod, or scope, contains a camera and a light. The scope lets the surgeon to see inside your wrist. He or she cuts the tissue using tiny surgical tools.
After the surgery, your hand and wrist are wrapped and put into a splint. This will help to keep you from moving your wrist during your recovery. You will need to wear the splint for a week or two. You will probably have some pain after your surgery. It’s usually controlled with pain medication taken by mouth. You may also be told to sleep with your hand elevated to help ease swelling.
Recovery from carpal tunnel surgery is different for each person. If your nerve has been compressed for a long time, recovery may take longer. You will be encouraged to move your fingers and wrist a few days after surgery to help prevent stiffness.
You may need to adjust your work or home activities while you recover. Talk with your healthcare provider about what you need to change.
 MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka
MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka