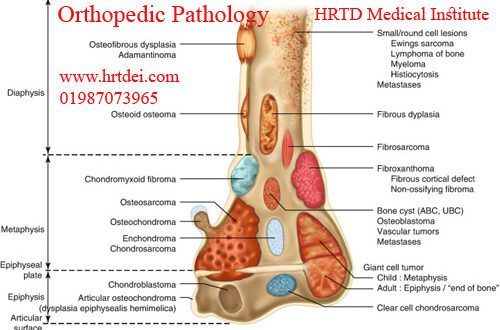
Orthopedic Pathology & Diagnosis Details
Orthopedic Pathology. Mobile Phone Number 01797522136, 01987073965. Orthopedic Pathology is a branch of pathology that discusses the causes and diagnosis of diseases in the musculoskeletal system. Diseases of Musculoskeletal Systems are called Orthopedic Diseases. These Diseases are Back Pain, Muscle cramps, Osteoporosis, Osteoarthritis, Rheumatoid Arthritis, Ankylosing Spondylitis, Muscle atrophy, Bursitis, Knee pain, Frozen shoulder, Shoulder arthritis, Dislocated shoulder,
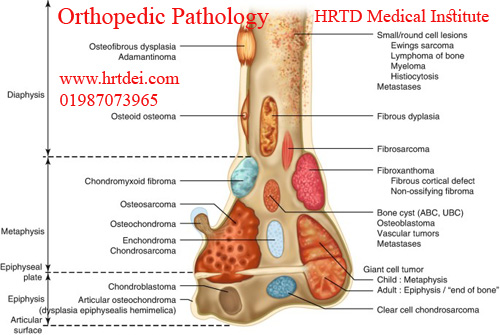
Fibromyalgia, Ankle sprains, Bone Fracture, Carpal tunnel syndrome, Acute injuries, Musculoskeletal cancer, Hip labral tear, Tennis elbow, Rotator cuff tear, Anterior cruciate ligament injury, Scoliosis, Rickets, etc. There are some courses for studying orthopedic diseases at HRTD Medical Institute. These Courses are DMA, DMS, DPM, DMDS, DMSc, and PDT Orthopedics. PDT Orthopedic is the best course for studying Orthopedic Diseases.
Causes and Diagnosis of Muscle Cramps
Causes of Muscle Cramps in Orthopedic Pathology
Muscle tissue relies, in part, on a range of minerals, electrolytes, and other chemicals in order to contract and relax. Some of these important substances include calcium, magnesium, potassium, and sodium. Inadequate diet, dehydration, vomiting, and diarrhea are just some of the factors that are thought to disturb the body’s balance of minerals and electrolytes and make muscles more susceptible to cramping.

Tetany is a special form of cramping – it can be brought on by over-breathing, which results in a low level of carbon dioxide in the blood. It is usually caused by anxiety.
Risk factors for muscle cramps
The exact cause of muscle cramp is not known, but risk factors may include:
- tight, inflexible muscles
- poor physical condition
- poor muscle tone
- inadequate diet
- physical overexertion
- physical exertion of cold muscles
- muscle injury
- muscle fatigue
- excessive perspiration
- dehydration – caused by, for example, a bout of gastroenteritis
- reduced blood supply (ischemia)
- wearing high-heeled shoes for lengthy periods.
Muscle cramps associated with medical conditions
Certain diseases or conditions may increase the risk of muscle cramps, including:
- Atherosclerosis – a condition characterized by narrowed arteries due to the formation of fatty plaques. Muscles are more likely to cramp if their blood supply is inadequate.
- Sciatica – pain in the buttock and leg caused by pressure on nerves in the lower back. In some cases, the irritated nerve may prompt the associated muscles to contract.
- Medications – some medical conditions require the regular use of fluid pills (diuretics). These drugs can interfere with the body’s mineral balance and contribute to cramping.
Causes of Osteoporosis in Orthopedic Pathology
In Orthopedic Pathology, Osteoporosis is a common orthopedic disease. Osteoporosis occurs when too much bone mass is lost and changes occur in the structure of bone tissue.
Bone is a living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Certain risk factors may lead to the development of osteoporosis.
Sex. Women have a greater risk for osteoporosis than men.
Age. As you age, bone loss happens more quickly, and new bone growth is slower.
Body size. Slender, thin-boned women and men are at greater risk of developing osteoporosis.
Skin Condition. White skin is at the highest risk.
Family history. The risk for osteoporosis and fractures may increase if one of your parents has a history of osteoporosis.
Changes to hormones. Low levels of certain hormones can increase osteoporosis. For example:
Low levels of estrogen in women ( during menopause).
Low levels of testosterone in men.
Diet. A diet low in calcium and vitamin D can increase your risk for osteoporosis and fractures.
Excessive dieting or poor protein intake may increase the risk of bone loss and osteoporosis.
Other medical conditions. Endocrine and hormonal diseases, gastrointestinal diseases, rheumatoid arthritis, certain types of cancer, HIV/AIDS, and anorexia nervosa.
Medications. Long-term use of certain medications:
Glucocorticoids and adrenocorticotropic hormone.
Antiepileptic medicines.
Cancer medications.
Proton pump inhibitors.
Selective serotonin reuptake inhibitors.
Thiazolidinediones, which treat type II diabetes.
Lifestyle.Low levels of physical activity.
Chronic heavy drinking of alcohol is a significant risk factor for osteoporosis.
Diagnosis of Osteoporosis is related to Orthopedic Pathology
In Orthopedic Pathology, Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of minerals in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only certain bones are checked — usually in the hip and spine.
Diagnosis of Osteoarthritis
There is no single test for osteoarthritis. Diagnosing the condition may include the following:
- Providing to a doctor a medical history that includes your symptoms, any other medical problems you and your close family members have, and any medications you are taking.
- Having a physical exam to check your general health, reflexes, and problem joints.
- Having images taken of your joint using: X-rays, which can show loss of joint space, bone damage, bone remodeling, and bone spurs.
- Having blood tests to rule out other causes for symptoms.
- Taking joint fluid samples to look for other causes of joint pain, such as infection or gout.
Treatment of Osteoarthritis
Treatment for osteoarthritis include:
- Reducing pain and other symptoms.
- Improving joint function.
- Stopping the disease from progressing.
- Maintaining a health-related quality of life to help prevent disability.
Symptoms of osteoarthritis, including:
- Oral pain relievers.
- Oral anti-inflammatory medications to treat pain and inflammation.
- Topical creams, rubs, or sprays that you apply to the skin over sore joints to relieve pain.
- Corticosteroids, strong inflammation-fighting drugs that are usually injected into the joint to temporarily relieve pain. Because they are potent drugs, your doctor will determine how many injections you should receive and how often to achieve the desired benefit.
- Hyaluronic acid substitutes (viscosupplements), which are injected into the knee to replace a normal component of the joint involved in lubrication and nutrition are sometimes recommended for knee osteoarthritis.
- Selective serotonin and norepinephrine reuptake inhibitors that you take orally to help control chronic (long-term) pain.
Causes of Osteoarthritis in Orthopedic Pathology
In Orthopedic Pathology, Osteoarthritis is a common orthopedic disease. Osteoarthritis are degenerative disease of the joint characterized by degeneration of articular cartilage with the proliferation of new bone and remodeling of joint contour. Commonly involves bearing joints- knee, ankle.
Causes of Gout is an Orthopedic Pathology
A buildup of excess uric acid in your body causes gout. Your body naturally makes uric acid when it breaks down chemicals called purines found in certain foods and drinks. Your kidneys usually filter uric acid out of your blood, and then it leaves your body when you pee. Sometimes your body makes too much uric acid, or your kidneys don’t remove it from your blood fast enough.
When your body has high levels of uric acid (hyperuricemia), uric acid crystals can build up and settle into your joints. The sharp crystals clump together and cause sudden episodes of pain, swelling, and other symptoms. Having temporarily high uric acid levels doesn’t mean you’ll definitely develop gout. Many people with hyperuricemia never get gout.
Gout risk factors are related to Orthopedic Pathology
Gout can affect anyone. People assigned male at birth (AMAB) are three times more likely to develop gout. People assigned female at birth (AFAB) usually don’t experience gout until after menopause. People with certain health conditions are more likely to develop gout, including:
- Overweight or obesity.
- Congestive heart failure.
- Diabetes.
- Hypertension (high blood pressure).
- Kidney disease.
- Blood cancer.
You’re more likely to experience gout if you:
- Have a biological parent or grandparent who has gout.
- Eat a lot of animal proteins — especially animal flesh, shellfish, and foods that contain organ meat.
- Drink alcohol regularly.
- Take a diuretic medication (water pills).
- Take immunosuppressants
Diagnosis of Gout is related to Orthopedic Pathology
A healthcare provider will diagnose gout with a physical exam. They’ll ask you about your symptoms and examine your affected joints. Tell your provider when you first notice symptoms like pain and swelling in your joint and how often the symptoms come and go.
Test for Diagnosis of Gout is a part of Orthopedic Pathology
Your healthcare provider might use a few imaging tests to take pictures of your affected joints. These tests can also show if gout has caused any changes in your joints. You might need:
- X-rays.
- Ultrasound.
- Magnetic resonance imaging (MRI).
- A CT (computed tomography) scan — specifically a dual-energy CT scan.
Other common tests to diagnose gout include:
- Blood tests to measure the uric acid in your blood.
- Joint aspiration — using a needle to remove a sample of fluid from inside a joint.
Causes and Diagnosis of Rheumatoid Arthritis
Causes of rheumatoid arthritis
The exact cause of rheumatoid arthritis is unknown. Researchers think it’s caused by a combination of genetics, hormones and environmental factors.
Normally, immune system protects your body from disease. With rheumatoid arthritis, something triggers of immune system to attack your joints. An infection, smoking or physical or emotional stress may be triggering.
Diagnostic criteria for rheumatoid arthritis
Diagnostic criteria are a set of signs, symptoms and test results your provider looks for before telling you that you’ve got rheumatoid arthritis. They’re based on years of research and clinical practice. Some people with RA don’t have all the criteria. Generally, though, the diagnostic criteria for rheumatoid arthritis include:
- Inflammatory arthritis in two or more large joints (shoulders, elbows, hips, knees and ankles).
- Inflammatory arthritis in smaller joints.
- Positive biomarker tests like rheumatoid factor (RF) or CCP antibodies.
- Elevated levels of CRP or an elevated sed rate.
Causes and Diagnosis of Ankylosing Spondylitis
Ankylosing Spondylitis Causes
Ankylosing Spondylitis is an autoimmune disease. These conditions happen when your body attacks its own immune system for some unknown reason. Researchers aren’t sure what triggers AS, but they think it’s tied to your genes. Most people with AS have a gene called HLA-B27. Doctors think that a mutation, or change, in this gene may be what causes AS.
Ankylosing Spondylitis Diagnosis
AS can be tough to spot because so many people have back pain, its main symptom.
Tests for ankylosing spondylitis
There’s no single test to confirm AS. Your doctor may rely on your symptoms as well as:
- A physical exam
- Blood tests to see if you have the HLA-B27
- An imaging test, such as an X-ray or MRI scan
Causes and Diagnosis of Bursitis
Causes of Bursitis
The most common causes of bursitis are repetitive motions or positions that put pressure on the bursae around a joint. Examples include:
- Throwing a baseball or lifting something over your head repeatedly
- Leaning on your elbows for long periods
- Extensive kneeling for tasks such as laying carpet or scrubbing floors
Risk factors of Bursitis
Anyone can develop bursitis, but certain factors can increase your risk:
- Age. Bursitis becomes more common with aging.
- Occupations or hobbies. If your work or hobby requires repetitive motion or pressure on particular bursae, your risk of developing bursitis increases. Examples include carpet laying, tile setting, gardening, painting and playing a musical instrument.
- Other medical conditions. Certain systemic diseases and conditions — such as rheumatoid arthritis, gout and diabetes — increase your risk of developing bursitis. Being overweight can increase your risk of developing hip and knee bursitis.
Diagnosis of Bursitis
Doctors can often diagnose bursitis based on a medical history and physical exam. Testing, if needed, might include:
- Imaging tests. X-ray images can’t positively establish the diagnosis of bursitis, but they can help to exclude other causes of your discomfort. Ultrasound or MRI might be used if your bursitis can’t easily be diagnosed by a physical exam alone.
- Lab tests. Your doctor might order blood tests or an analysis of fluid from the inflamed bursa to pinpoint the cause of your joint inflammation and pain.
Causes and Diagnosis of Knee Pain
Causes of Knee Pain
Knee pain can have different causes. Being overweight puts you at greater risk for knee problems. Overusing your knee can trigger knee problems that cause pain. If you have a history of arthritis, it could also cause knee pain.
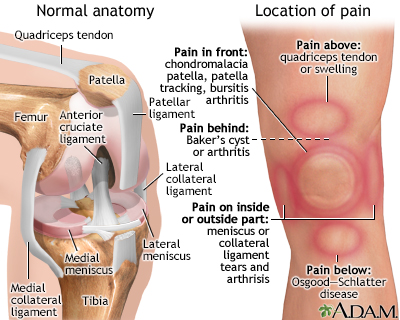
Here are some common causes of knee pain:
MEDICAL CONDITIONS
- Arthritis — Including rheumatoid arthritis, osteoarthritis, lupus, and gout
- Baker cyst — A fluid-filled swelling behind the knee that may occur with swelling (inflammation) from other causes, such as arthritis
- Cancers that either spread to your bones or begin in the bones
- Osgood-Schlatter disease
- Infection in the bones around the knee
- Infection in the knee joint
Diagnosis
During the physical exam, your doctor is likely to:
- Inspect your knee for swelling, pain, tenderness, warmth and visible bruising
- Check to see how far you can move your lower leg in different directions
- Push on or pull the joint to evaluate the integrity of the structures in your knee
Causes and Diagnosis of Frozen Shoulder
Causes of Frozen Shoulder is a part of Orthopedic Pathology
A capsule of connecting tissue encases the shoulder joint. When these connecting tissues become thicker and tighter, the movement of the shoulder is restricted. The reason why the tissues get thicken and tighten is still unclear. However, systemic diseases and immobilizing the shoulder for a long period, such as in people after surgery or arm fracture tend to be involved in developing this condition.
Diagnosis of Frozen Shoulder is related to Orthopedic Pathology
The doctor may conduct a physical exam to check for the pain and evaluate an active and passive range of motion since either of them can be affected. A numbing medicine might be injected in some cases. Normally, a frozen shoulder can be diagnosed by a physical exam and review of signs and symptoms. However, to seek for other problems, the doctor may be required to use some image tests, such as X-rays or MRI.
Causes and Diagnosis of Muscle Atrophy
Causes of muscle atrophy is a part of Orthopedic Pathology
The cause of muscle atrophy depends on the type you have. Disuse (physiologic) atrophy is caused by not using your muscles enough. If you stop using your muscles, your body won’t waste the energy it needs to take care of them. Instead, your body will start to break your muscles down, which causes them to decrease in size and strength. Disuse atrophy may affect you if you:
Lead a sedentary lifestyle.
Are malnourished.
Don’t get enough exercise.
Sit at a desk job all day.
Are on best rest.
Have a genetic disorder such as muscular dystrophy or Charcot-Marie-Tooth disease.
Can’t move your limbs due to a stroke or other conditions such as dermatomyositis.
Have age-related atrophy (sarcopenia).
Neurogenic atrophy is caused by an injury or disease affecting nerves that connect to your muscles. When these nerves are damaged, they can’t trigger the muscle contractions that are needed to stimulate muscle activity. When your muscles don’t contract, your body thinks you don’t need them anymore. So your body starts breaking them down, which causes them to decrease in size and strength. Diseases and other conditions that can affect these nerves include:
Amyotrophic lateral sclerosis (ALS).
Diagnosis and Tests of Muscle Atrophy is a part of Orthopedic Pathology
To diagnose muscle atrophy, your healthcare provider will give you a physical exam and ask you about your symptoms. They’ll look at your arms and legs and measure your muscle mass. In addition, your healthcare provider may order tests, including:
Muscle or nerve biopsy.
Nerve conduction studies.
X-rays.
Computed tomography (CT) scan.
Magnetic resonance imaging (MRI) scan.
Causes and Diagnosis of Shoulder Arthritis
Causes of shoulder arthritis?
Shoulder arthritis has many possible causes. They include:
- Osteoarthritis: This is the most common type of arthritis. This is the “wear and tear,” age-related type of joint disease. Cartilage gets soft, cracks, flakes or becomes frayed and eventually wears away.
- Rheumatoid arthritis:This is an autoimmune disease, which means your body’s defense system attacks its own healthy tissues.
- Rotator cuff tear arthropathy: The rotator cuff is a group of four tendons that surround your shoulder joint and keep your shoulder stable as the “ball” of your upper arm rotates in your shoulder blade socket during movement. Tearing of these tendons (rotator cuff tears) usually happens as slow fraying and wearing over time.
- Trauma to your shoulder: Any type of injury to the bones of the shoulder — including dislocation, fracture or severe impact — can damage the cartilage surface.
- Avascular necrosis: This condition, also called osteonecrosis, is the death of part of the “ball” of your shoulder. Trauma or disease cut off blood flow to the bone. Without bone support, the cartilage becomes damaged and eventually, the shoulder joint breaks down.
Diagnosis of shoulder arthritis
Your healthcare provider will perform a physical exam of your shoulder, including checking the range of motion and strength. Your provider will also ask about your medical history and current symptoms.
Your provider will order imaging tests, including:
- X-rays: X-rays show the condition of your shoulder bones. They can’t directly show cartilage, but your provider can see the amount of space between your shoulder bones. Being very close or touching means you’ve lost cartilage.
- Computed tomography (CT) scan: This test provides more detail of the bones of your shoulder joint than X-rays and is frequently ordered for surgical planning
- Magnetic resonance imaging (MRI): This test shows the surrounding soft tissues of your shoulder joint. Your provider may order it to look at the condition of the rotator cuff tendons.
Causes and Diagnosis of Dislocated Shoulder
Causes of shoulder dislocations
Any force that’s strong enough to push your shoulder joint out of place can cause a dislocation. The most common causes include:
- Falls.
- Car accidents.
- Sports injuries.
Dislocated shoulder risk factors
Anyone can experience a shoulder dislocation, but some people have a higher risk than others, including:
- Athletes who play contact sports.
- Men and people assigned male at birth (AMAB).
- People between 15 and 30 years old.
- Anyone who has previously dislocated their shoulder.
Diagnosis of dislocated shoulder
Your provider might need some of the following imaging tests to diagnose damage inside your body after a dislocation:
Causes and Diagnosis of Fibromyalgia
What causes fibromyalgia?
Experts don’t know what causes fibromyalgia.
Certain genes you inherit from your biological parents might make you more likely to develop fibromyalgia. Studies have found a link between biological parents who have fibromyalgia and their children — this might mean it’s passed down through families.
People with fibromyalgia are usually more sensitive to pain than most people. Experts haven’t found the direct link yet, but they think genetic mutations in the genes responsible for forming the neurotransmitters in your brain that broadcast and receive pain signals to your body might cause fibromyalgia.
What are the risk factors for fibromyalgia?
Even though experts can’t say for sure what causes fibromyalgia, some health conditions and other issues are risk factors for developing it. Fibromyalgia risk factors include:
- Your age: People older than 40 are more likely to develop fibromyalgia. But it can affect anyone, including children.
- Your sex assigned at birth: People assigned female at birth are twice as likely to experience fibromyalgia.
- Chronic illnesses: People with conditions like osteoarthritis, depression, anxiety disorders, chronic back pain, and irritable bowel syndrome are more likely to develop fibromyalgia.
- Infections: Some people develop fibromyalgia after having an infection, especially if they experience severe symptoms.
- Stress: The amount of stress you experience can’t be measured on a test, but too much stress can affect your health.
- Traumas: People who’ve experienced a physical or emotional trauma or a serious injury sometimes develop fibromyalgia.
Causes and Diagnosis of Bone Fracture
Causes of bone fractures
Causes of bone fractures can include:
- traumatic incidents such as sporting injuries, vehicle accidents, and falls
- conditions such as osteoporosis and some types of cancer that cause bones to fracture more easily, meaning even minor trauma and falls can become serious.
Diagnosis of bone fractures
Doctors can diagnose bone fractures with X-rays. They may also use CT scans (computed tomography) and MRI scans (magnetic resonance imaging).
 MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka
MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka