Orthopedic Diseases-2 Details
Orthopedic Disease-2. Mobile Phone Number. 01797522136, 01987073965. In Orthopedic Medicines-1 We have discussed the diseases Low back pain, Osteoporosis, Arthritis, Gout, Frozen Shoulder, Muscle atrophy, Bone Fracture, Muscle cramps, Fibromyalgia, and Carpal Tunnel Syndrome.

In Orthopedic Diseases-2 we will discuss some diseases that are not mentioned in Orthopedic Disease-1. These Orthopedic Diseases are Ankylosing Spondylitis, Bursitis, Knee pain, Shoulder arthritis, Dislocated shoulder, Ankle sprains, Acute injuries, Musculoskeletal cancer, Hip labral tear, Tennis elbow, Rotator cuff tear, Anterior cruciate ligament injury, Scoliosis, Rickets, etc. We can study Orthopedic Disease in PDT Orthopedic Courses. These courses are PDT Orthopedics 6 Months, PDT Orthopedics 1 Year, and PDT Orthopedics 2 Years. All these courses are available at HRTD Medical Institute.
Students can study PDT Orthopedic Courses after completing the Diploma Medical Courses of Long and Short Duration. Diploma Medical Courses are DMF, DMA 3 Years, DMA 2 Years, DMA 1 Year, DMS 3 Years, DMS 2 Years, DMS 1 Year, DMDS 4 Years, etc. All the Diploma Courses are available at HRTD Medical Institute. You must have a science background for the DMF course and any background (But minimum SSC Pass) for other medical diploma courses.
Ankylosing Spondylitis in Orthopedic Disease-2
Inflammation of the joints and ligaments of the spine is called Ankylosing Spondylitis. Ankylosing spondylitis is a type of arthritis. It may also affect peripheral joints like the knees, ankles, and hips. Normally, the joints and ligaments in the spine help us move and bend. If we have ankylosing spondylitis, the inflammation in the joints and tissues of the spine can cause stiffness. This may cause the vertebrae to fuse (grow together) in severe cases. When the vertebrae fuse, it can lead to a rigid and inflexible spine.
Factors of getting/developing Ankylosing Spondylitis
Factors of getting/developing Ankylosing Spondylitis:
- Family history and genetics. If you have a family history of ankylosing spondylitis, you are more likely to develop the disease.
- Age. Most people develop symptoms of ankylosing spondylitis before age 45. However, some people develop the disease when they are children or teens.
- Some diseases. People who have Crohn’s disease, ulcerative colitis, or psoriasis may be more likely to develop the disease.
Symptoms of Ankylosing Spondylitis
Early symptoms of ankylosing spondylitis might include back pain and stiffness in the lower back and hips, especially in the morning and after periods of inactivity. Neck pain and fatigue also are common. Over time, symptoms might worsen, improve, or stop at irregular intervals.
The areas most commonly affected are:
- The joint between the base of the spine and the pelvis.
- The vertebrae in the lower back.
- The places where tendons and ligaments attach to bones, mainly in the spine, but sometimes along the back of the heel.
- The cartilage between the breastbone and the ribs.
- The hip and shoulder joints.
Causes of Ankylosing Spondylitis
Ankylosing spondylitis has no known specific cause, though genetic factors seem to be involved. In particular, people who have a gene called HLA-B27 are at a greatly increased risk of developing ankylosing spondylitis. However, only some people with the gene develop the condition.
Complications of Ankylosing Spondylitis
In severe ankylosing spondylitis, new bone forms as part of the body’s attempt to heal. This new bone gradually bridges the gap between vertebrae and eventually fuses sections of vertebrae. Those parts of the spine become stiff and inflexible. Fusion also can stiffen the rib cage, restricting lung capacity and function.
Other complications might include:
- Eye inflammation, called uveitis. One of the most common complications of ankylosing spondylitis, uveitis can cause rapid-onset eye pain, sensitivity to light, and blurred vision. See your healthcare provider right away if you develop these symptoms.
- Compression fractures. Some people’s bones weaken during the early stages of ankylosing spondylitis. Weakened vertebrae can crumple, increasing the severity of a stooped posture. Vertebral fractures can put pressure on and possibly injure the spinal cord and the nerves that pass through the spine.
- Heart problems. Ankylosing spondylitis can cause problems with the aorta. The inflamed aorta can enlarge to the point that it distorts the shape of the aortic valve, which impairs its function. The inflammation associated with ankylosing spondylitis increases the risk of heart disease in general.
Diagnosis of Ankylosing Spondylitis
During the physical exam:
To bend in different directions to test the range of motion in the spine.
To reproduce pain by pressing on specific portions of the pelvis
To produce pain by moving the legs into a particular position.
Take a deep breath to see the difficulty expanding the chest.
Imaging tests
X-rays allow doctors to check for changes in joints and bones, also called radiographic axial spondyloarthritis, though the visible signs of ankylosing spondylitis, also called axial spondyloarthritis, might not be evident early in the disease.
Magnetic resonance imaging (MRI) uses radio waves and a strong magnetic field to provide more detailed images of bones and soft tissues. MRI scans can reveal evidence of non-radiographic axial spondyloarthritis earlier in the disease process, but they are much more expensive.
Lab tests
There are no specific lab tests to identify ankylosing spondylitis. Certain blood tests can check for markers of inflammation, but many different health problems can cause inflammation.
Blood can be tested for the HLA-B27 gene. However many people who have the gene don’t have ankylosing spondylitis, and people can have the disease without having the HLA-B27 gene.
Treatment of Ankylosing Spondylitis
The goal of treatment is to relieve pain and stiffness and prevent or delay complications and spinal deformity. Ankylosing spondylitis treatment is most successful before the disease causes irreversible damage.
Medications Treatment of Ankylosing Spondylitis
Nonsteroidal anti-inflammatory drugs (NSAIDs) — such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others) — are the medicines health care providers most commonly use to treat axial spondyloarthritis and nonradiographic axial spondyloarthritis. These medicines can relieve inflammation, pain, and stiffness, but they also might cause gastrointestinal bleeding.
If nonsteroidal anti-inflammatory drugs (NSAIDs) aren’t helpful, your doctor might suggest starting a tumor necrosis factor (TNF) blocker or an interleukin-17 (IL-17) inhibitor. These medicines are injected under the skin or through an intravenous line. Another option is a Janus kinase (JAK) inhibitor. Janus kinase (JAK) inhibitors are taken by mouth. These types of medicines can reactivate untreated tuberculosis and make you more prone to infections.
Examples of tumor necrosis factor (TNF) blockers include:
- Adalimumab (Humira).
- Certolizumab pegol (Cimzia).
- Etanercept (Enbrel).
- Golimumab (Simponi).
- Infliximab (Remicade).
Interleukin-17 (IL-17) inhibitors used to treat ankylosing spondylitis include secukinumab (Cosentyx). Janus kinase (JAK) inhibitors available to treat ankylosing spondylitis include tofacitinib (Xeljanz) and upadacitinib (Rinvoq).
Therapy Treatment of Ankylosing Spondylitis
Physical therapy is an important part of treatment and can provide a number of benefits, from pain relief to improved strength and flexibility. A physical therapist can design specific exercises for your needs. To help preserve good posture, you may be taught:
- Range-of-motion and stretching exercises.
- Strengthening exercises for abdominal and back muscles.
- Proper sleeping and walking positions.
Surgery Treatment of Ankylosing Spondylitis
Most people with ankylosing spondylitis or nonradiographic axial spondyloarthritis don’t need surgery. Surgery may be recommended if you have severe pain or if a hip joint is so damaged that it needs to be replaced.
Bursitis in Orthopedic Disease-2
Bursitis is a painful condition that affects the small, fluid-filled sacs — called bursae (bur-SEE) — that cushion the bones, tendons, and muscles near your joints. Bursitis occurs when bursae become inflamed.
The most common locations for bursitis are in the shoulder, elbow, and hip. But you can also have bursitis by your knee, heel, and the base of your big toe. Bursitis often occurs near joints that perform frequent repetitive motion.
Treatment typically involves resting the affected joint and protecting it from further trauma. In most cases, bursitis pain goes away within a few weeks with proper treatment, but recurrent flare-ups of bursitis are common.
Symptoms of Bursitis
If you have bursitis, the affected joint might:
- Feel achy or stiff
- Hurt more when you move it or press on it
- Look swollen and red
Causes of Bursitis
The most common causes of bursitis are repetitive motions or positions that put pressure on the bursae around a joint. Examples include:
- Throwing a baseball or lifting something over your head repeatedly
- Leaning on your elbows for long periods
- Extensive kneeling for tasks such as laying carpet or scrubbing floors
Other causes include injury or trauma to the affected area, inflammatory arthritis such as rheumatoid arthritis, gout, and infection.
Risk factors of Bursitis
Anyone can develop bursitis, but certain factors can increase your risk:
- Age. Bursitis becomes more common with aging.
- Occupations or hobbies. If your work or hobby requires repetitive motion or pressure on particular bursae, your risk of developing bursitis increases. Examples include carpet laying, tile setting, gardening, painting, and playing a musical instrument.
- Other medical conditions. Certain systemic diseases and conditions — such as rheumatoid arthritis, gout, and diabetes — increase your risk of developing bursitis. Being overweight can increase your risk of developing hip and knee bursitis.
Prevention of Bursitis
While not all types of bursitis can be prevented, you can reduce your risk and the severity of flare-ups by changing the way you do certain tasks. Examples include:
- Using kneeling pads. Use some type of padding to reduce the pressure on your knees if your job or hobby requires a lot of kneeling.
- Lifting properly. Bend your knees when you lift. Failing to do so puts extra stress on the bursae in your hips.
- Wheeling heavy loads. Carrying heavy loads puts stress on the bursae in your shoulders. Use a dolly or a wheeled cart instead.
- Taking frequent breaks. Alternate repetitive tasks with rest or other activities.
- Maintaining a healthy weight. Being overweight places more stress on your joints.
- Exercising. Strengthening your muscles can help protect your affected joints.
- Warm up and stretch before strenuous activities to protect your joints from injury.
Diagnosis of Bursitis
Doctors can often diagnose bursitis based on a medical history and physical exam. Testing, if needed, might include:
- Imaging tests. X-ray images can’t positively establish the diagnosis of bursitis, but they can help to exclude other causes of your discomfort. Ultrasound or MRI might be used if your bursitis can’t easily be diagnosed by a physical exam alone.
- Lab tests. Your doctor might order blood tests or an analysis of fluid from the inflamed bursa to pinpoint the cause of your joint inflammation and pain.
Treatment of Bursitis
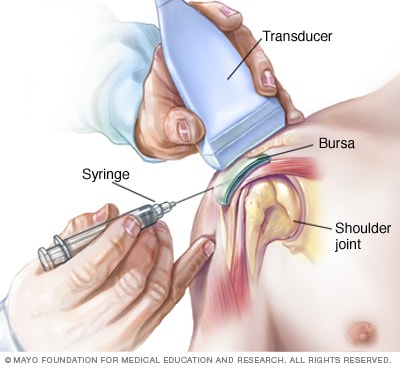
Shoulder injectionEnlarge image
Bursitis generally gets better on its own. Conservative measures, such as rest, ice, and taking a pain reliever, can relieve discomfort. If conservative measures don’t work, you might require:
- Medication. If the inflammation in your bursa is caused by an infection, your doctor might prescribe an antibiotic.
- Therapy. Physical therapy or exercises can strengthen the muscles in the affected area to ease pain and prevent recurrence.
- Injections. A corticosteroid drug injected into the bursa can relieve pain and inflammation in your shoulder or hip. This treatment generally works quickly.
- Assistive device. Temporary use of a walking cane or other device will help relieve pressure on the affected area.
- Surgery. Sometimes an inflamed bursa must be surgically drained, but only rarely is surgical removal of the affected bursa necessary.
Lifestyle Modification and OTC Drugs Application
Measures you can take to relieve the pain of bursitis include:
- Rest and don’t overuse the affected area.
- Apply ice to reduce swelling for the first 48 hours after symptoms occur.
- Apply dry or moist heat, such as a heating pad, or take a warm bath.
- Take an over-the-counter medication, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others), to relieve pain and reduce inflammation. Some are available in a form you apply to the skin.
- Cushion your knees if you sleep on your side by placing a small pillow between your legs.
Knee Pain in Orthopedic Disease-2
Knee pain is a common complaint that affects people of all ages. Knee pain may be the result of an injury, such as a ruptured ligament or torn cartilage. Medical conditions — including arthritis, gout, and infections — also can cause knee pain.
Many types of minor knee pain respond well to self-care measures. Physical therapy and knee braces also can help relieve pain. In some cases, however, your knee may require surgical repair.
Symptoms of Knee Pain
The location and severity of knee pain may vary, depending on the cause of the problem. Signs and symptoms that sometimes accompany knee pain include:
- Swelling and stiffness
- Redness and warmth to the touch
- Weakness or instability
- Popping or crunching noises
- Inability to fully straighten the knee
Causes of Knee Pain
Knee pain can be caused by injuries, mechanical problems, types of arthritis, and other problems.
Injuries
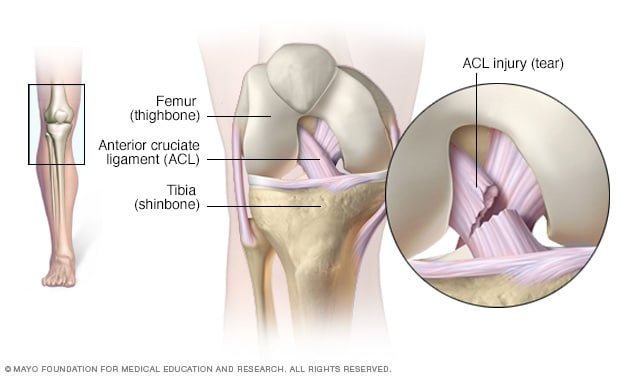 ACL injuryEnlarge image
ACL injuryEnlarge image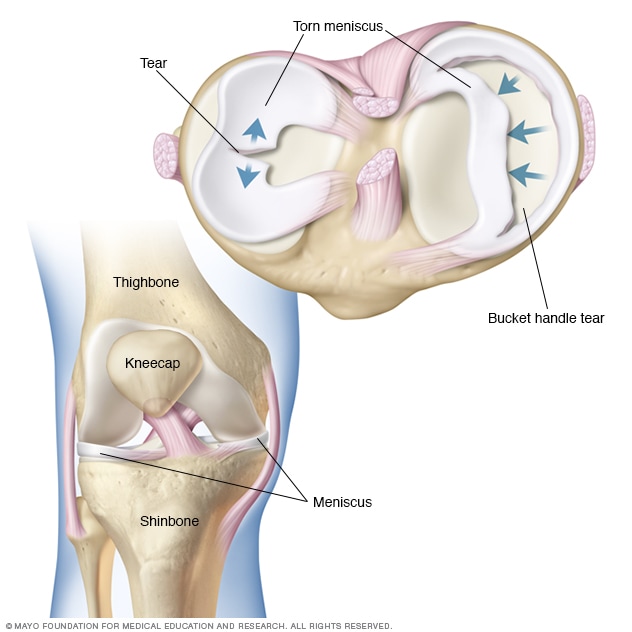 Torn meniscusEnlarge image
Torn meniscusEnlarge image
A knee injury can affect any of the ligaments, tendons, or fluid-filled sacs (bursae) that surround your knee joint as well as the bones, cartilage, and ligaments that form the joint itself. Some of the more common knee injuries include:
- ACL injury. An ACL injury is a tear of the anterior cruciate ligament (ACL) — one of four ligaments that connect your shinbone to your thighbone. An ACL injury is particularly common in people who play basketball, soccer, or other sports that require sudden changes in direction.
- Fractures. The bones of the knee, including the kneecap (patella), can be broken during falls or auto accidents. Also, people whose bones have been weakened by osteoporosis can sometimes sustain a knee fracture simply by stepping wrong.
- Torn meniscus. The meniscus is the tough, rubbery cartilage that acts as a shock absorber between your shinbone and thighbone. It can be torn if you suddenly twist your knee while bearing weight on it.
- Knee bursitis. Some knee injuries cause inflammation in the bursae, the small sacs of fluid that cushion the outside of your knee joint so that tendons and ligaments glide smoothly over the joint.
- Patellar tendinitis. Tendinitis causes irritation and inflammation of one or more tendons — the thick, fibrous tissues that attach muscles to bones. This inflammation can happen when there’s an injury to the patellar tendon, which runs from the kneecap (patella) to the shinbone and allows you to kick, run, and jump. Runners, skiers, cyclists, and those involved in jumping sports and activities may develop patellar tendinitis.
Mechanical problems
Some examples of mechanical problems that can cause knee pain include:
- Loose body. Sometimes injury or degeneration of bone or cartilage can cause a piece of bone or cartilage to break off and float in the joint space. This may not create any problems unless the loose body interferes with knee joint movement, in which case the effect is something like a pencil caught in a door hinge.
- Iliotibial band syndrome. This occurs when the tough band of tissue that extends from the outside of your hip to the outside of your knee (iliotibial band) becomes so tight that it rubs against the outer portion of your thighbone. Distance runners and cyclists are especially susceptible to iliotibial band syndrome.
- Dislocated kneecap. This occurs when the triangular bone that covers the front of your knee (patella) slips out of place, usually to the outside of your knee. In some cases, the kneecap may stay displaced and you’ll be able to see the dislocation.
- Hip or foot pain. If you have hip or foot pain, you may change the way you walk to spare your painful joint. However, this altered gait can place more stress on your knee joint and cause knee pain.
Arthritis that Affects the Knee
More than 100 different types of arthritis exist. The varieties most likely to affect the knee include:
- Osteoarthritis. Sometimes called degenerative arthritis, osteoarthritis is the most common type of arthritis. It’s a wear-and-tear condition that occurs when the cartilage in your knee deteriorates with use and age.
- Rheumatoid arthritis. The most debilitating form of arthritis, rheumatoid arthritis is an autoimmune condition that can affect almost any joint in your body, including your knees. Although rheumatoid arthritis is a chronic disease, it tends to vary in severity and may even come and go.
- Gout. This type of arthritis occurs when uric acid crystals build up in the joint. While gout most commonly affects the big toe, it can also occur in the knee.
- Pseudogout. Often mistaken for gout, pseudogout is caused by calcium-containing crystals that develop in the joint fluid. The knees are the most common joint affected by pseudogout.
- Septic arthritis. Sometimes your knee joint can become infected, leading to swelling, pain, and redness. Septic arthritis often occurs with a fever, and there’s usually no trauma before the onset of pain. Septic arthritis can quickly cause extensive damage to the knee cartilage. If you have knee pain with any of the symptoms of septic arthritis, see your doctor right away.
Risk factors for knee problems
Many factors can increase your risk of having knee problems, including:
- Excess weight. Being overweight or obese increases stress on your knee joints, even during ordinary activities such as walking or going up and down stairs. It also puts you at increased risk of osteoarthritis by accelerating the breakdown of joint cartilage.
- Lack of muscle flexibility or strength. A lack of strength and flexibility can increase the risk of knee injuries. Strong muscles help stabilize and protect your joints, and muscle flexibility can help you achieve a full range of motion.
- Certain sports or occupations. Some sports put greater stress on your knees than others. Alpine skiing with its rigid ski boots and potential for falls, basketball’s jumps and pivots, and the repeated pounding your knees take when you run or jog all increase your risk of a knee injury. Jobs that require repetitive stress on the knees such as construction or farming also can increase your risk.
- Previous injury. Having a previous knee injury makes it more likely that you’ll injure your knee again.
Complications of knee problems
Not all knee pain is serious. However, some knee injuries and medical conditions, such as osteoarthritis, can lead to increasing pain, joint damage, and disability if left untreated. And having a knee injury — even a minor one — makes it more likely that you’ll have similar injuries in the future.
Prevention of Knee Problems
Although it’s not always possible to prevent knee pain, the following suggestions may help ward off injuries and joint deterioration:
- Keep extra pounds off. Maintain a healthy weight; it’s one of the best things you can do for your knees. Every extra pound puts additional strain on your joints, increasing the risk of injuries and osteoarthritis.
- Be in shape to play your sport. To prepare your muscles for the demands of sports participation, take time for conditioning.
- Practice perfectly. Make sure the technique and movement patterns you use in your sports or activity are the best they can be. Lessons from a professional can be very helpful.
- Get strong, stay flexible. Weak muscles are a leading cause of knee injuries. You’ll benefit from building up your quadriceps and hamstrings, the muscles on the front and back of your thighs that help support your knees. Balance and stability training helps the muscles around your knees work together more effectively. And because tight muscles also can contribute to injury, stretching is important. Try to include flexibility exercises in your workouts.
- Be smart about exercise. If you have osteoarthritis, chronic knee pain, or recurring injuries, you may need to change the way you exercise. Consider switching to swimming, water aerobics, or other low-impact activities — at least for a few days a week. Sometimes simply limiting high-impact activities will provide relief.
Diagnosis of Knee Pain
During the physical exam, your doctor is likely to:
- Inspect your knee for swelling, pain, tenderness, warmth, and visible bruising
- Check to see how far you can move your lower leg in different directions
- Push on or pull the joint to evaluate the integrity of the structures in your knee
Imaging tests
In some cases, your doctor might suggest tests such as:
- X-ray. Your doctor may first recommend having an X-ray, which can help detect bone fractures and degenerative joint disease.
- Computerized tomography (CT) scan. CT scanners combine X-rays taken from many different angles to create cross-sectional images of the inside of your body. CT scans can help diagnose bone problems and subtle fractures. A special kind of CT scan can accurately identify gout even when the joint is not inflamed.
- Ultrasound. This technology uses sound waves to produce real-time images of the soft tissue structures within and around your knee. Your doctor may want to move your knee into different positions during the ultrasound to check for specific problems.
- Magnetic resonance imaging (MRI). An MRI uses radio waves and a powerful magnet to create 3D images of the inside of your knee. This test is particularly useful in revealing injuries to soft tissues such as ligaments, tendons, cartilage, and muscles.
Lab Tests for Knee Pain
If your doctor suspects an infection or inflammation, you’re likely to have blood tests and sometimes a procedure called arthrocentesis, in which a small amount of fluid is removed from within your knee joint with a needle and sent to a laboratory for analysis.
Treatment of Knee Pain
Treatments will vary, depending on what exactly is causing your knee pain.
Medications for knee pain
Your doctor may prescribe medications to help relieve pain and to treat the conditions causing your knee pain, such as rheumatoid arthritis or gout.
Therapy for Knee Pain
If you are physically active or practice a sport, you may need exercises to correct movement patterns that may be affecting your knees and to establish good technique during your sport or activity. Exercises to improve your flexibility and balance also are important.
Strengthening the muscles around your knee will make it more stable. Your doctor may recommend physical therapy or different types of strengthening exercises based on the specific condition that is causing your pain.
Arch supports, sometimes with wedges on one side of the heel, can help shift pressure away from the side of the knee most affected by osteoarthritis. In certain conditions, different types of braces may be used to help protect and support the knee joint.
Injections for Knee Pain
In some cases, your doctor may suggest injecting medications or other substances directly into your joint. Examples include:
- Corticosteroids. Injections of a corticosteroid drug into your knee joint may help reduce the symptoms of an arthritis flare and provide pain relief that may last a few months. These injections aren’t effective in all cases.
- Hyaluronic acid. A thick fluid, similar to the fluid that naturally lubricates joints, hyaluronic acid can be injected into your knee to improve mobility and ease pain. Although study results have been mixed about the effectiveness of this treatment, relief from one or a series of shots may last as long as six months.
- Platelet-rich plasma (PRP). PRP contains a concentration of many different growth factors that appear to reduce inflammation and promote healing. Some studies have found that PRP may benefit certain people with osteoarthritis, but more studies are needed.
Surgery for Knee Pain
If you have an injury that may require surgery, it’s usually not necessary to have the operation immediately. Before making a decision, consider the pros and cons of both nonsurgical rehabilitation and surgical reconstruction in relation to what’s most important to you. If you choose to have surgery, your options may include:
- Arthroscopic surgery. Depending on your injury, your doctor may be able to examine and repair your joint damage using a fiber-optic camera and long, narrow tools inserted through just a few small incisions around your knee. Arthroscopy may be used to remove loose bodies from your knee joint, remove or repair damaged cartilage (especially if it is causing your knee to lock), and reconstruct torn ligaments.
- Partial knee replacement surgery. In this procedure, your surgeon replaces only the most damaged portion of your knee with parts made of metal and plastic. The surgery can usually be performed through small incisions, so you’re likely to heal more quickly than you are with surgery to replace your entire knee.
- Total knee replacement. In this procedure, your surgeon cuts away damaged bone and cartilage from your thighbone, shinbone, and kneecap and replaces it with an artificial joint made of metal alloys, high-grade plastics, and polymers.
- Osteotomy. This procedure involves removing bone from the thighbone or shinbone to better align the knee and relieve arthritis pain. This surgery may help you delay or avoid total knee replacement surgery.
Lifestyle Modification and OTC Drugs Application
Over-the-counter medications — such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) — may help ease knee pain.
Some people find relief by rubbing the affected knee with creams containing a numbing agent, such as lidocaine, or capsaicin, the substance that makes chili peppers hot.
Self-care measures for an injured knee include:
- Rest. Take a break from your normal activities to reduce repetitive strain on your knee, give the injury time to heal, and help prevent further damage. A day or two of rest may be all you need for a minor injury. More severe damage is likely to need a longer recovery time.
- Ice. Ice reduces both pain and inflammation. A bag of frozen peas works well because it covers your whole knee. You also can use an ice pack wrapped in a thin towel to protect your skin. Although ice therapy is generally safe and effective, don’t use ice for longer than 20 minutes at a time because of the risk of damage to your nerves and skin.
- Heat. You may experience temporary pain relief by applying a heat pack or hot water bottle to the painful area on your knee.
- Compression. This helps prevent fluid buildup in damaged tissues and maintains knee alignment and stability. Look for a compression bandage that’s lightweight, breathable, and self-adhesive. It should be tight enough to support your knee without interfering with circulation.
- Elevation. To help reduce swelling, try propping your injured leg on pillows or sitting in a recliner.
Shoulder Arthritis
What is shoulder arthritis?
Shoulder arthritis is inflammation in your shoulder joint. The inflammation causes pain and stiffness. It makes lifting your arm uncomfortable.
The main joint of your shoulder is a “ball and socket” joint. It’s where the “ball” of your upper arm (humerus) rests against the “socket,” or hollowed-out cup, on the edge of your shoulder blade (scapula). This joint is called the glenohumeral joint.
Shoulder arthritis can also happen at a second joint in your shoulder where your collarbone (clavicle) meets the acromion on your shoulder blade. This joint is called the acromioclavicular joint or AC joint.
Over time, arthritis leads to cartilage loss. Cartilage is the tissue that covers the humeral head and the “socket” of your shoulder joint. Cartilage allows the bone surfaces to glide within the joint. It also cushions your bones against impact.
In the end stage of shoulder arthritis, without protective cartilage, bones in the joint rub directly against each other.
Causes of Shoulder Arthritis
- Osteoarthritis: This is the most common type of arthritis. This is the “wear and tear,” age-related type of joint disease. Cartilage gets soft, cracks, flakes or becomes frayed and eventually wears away. This exposes the bones beneath the cartilage, which begin to rub or grind against each other. Like the tires on your car, joint surfaces don’t wear down evenly or at the same rate.
- Rheumatoid arthritis: This is an autoimmune disease, which means your body’s defense system attacks its own healthy tissues. In rheumatoid arthritis of your shoulder, your immune system attacks the joint and joint lining, causing the lining to swell. The disease process eventually damages the cartilage.
- Rotator cuff tear arthropathy: The rotator cuff is a group of four tendons that surround your shoulder joint and keep your shoulder stable as the “ball” of your upper arm rotates in your shoulder blade socket during movement. Tearing of these tendons (rotator cuff tears) usually happens as slow fraying and wearing over time. In some instances, these tears can slowly become very larger over time, to the point that the humeral head slides out of its normal position and rubs against other shoulder bones, leading to cartilage wear and arthritis
- Trauma to your shoulder: Any type of injury to the bones of the shoulder — including dislocation, fracture, or severe impact — can damage the cartilage surface.
- Avascular necrosis: This condition, also called osteonecrosis, is the death of part of the “ball” of your shoulder. Trauma or disease cut off blood flow to the bone. Without bone support, the cartilage becomes damaged and eventually, the shoulder joint breaks down.
Symptoms of Shoulder Arthritis
Symptoms of shoulder arthritis vary from person to person. Signs and symptoms include:
- Pain in your shoulder joint: This is the most common symptom. At first, you may feel shoulder pain only during activity. Later in the disease process, you may feel pain at any time of the day, with or without arm movement. Your pain may worsen when you lift heavy objects or after exercise. The pain may spread down your arm and even to your elbow or wrist if your arthritis is severe.
- Stiffness and loss of range of motion: You may feel stiffness in your shoulder and lose range of motion. These symptoms may make everyday tasks — such as dressing, bathing, driving, or doing housework — difficult.
- Grinding, clicking, popping, or cracking in your shoulder joint: Loss of cartilage, which leaves an unsmooth surface, causes these noises. The noises occur with or without pain.
- Loss of sleep: It’s difficult to find a comfortable sleeping position. Any shoulder movement may cause pain. If you sleep on your back, place a pillow under the elbow of your affected side. This helps keep your shoulder in a more supported position. It also takes the strain off of all supporting joint structures. For some people, sleeping in a recliner can provide pain relief at night.
Diagnosis of Shoulder Arthritis
X-rays: X-rays show the condition of your shoulder bones. They can’t directly show cartilage, but your provider can see the amount of space between your shoulder bones. Being very close or touching means you’ve lost cartilage.
Computed tomography (CT) scan: This test provides more detail of the bones of your shoulder joint than X-rays and is frequently ordered for surgical planning
Magnetic resonance imaging (MRI): This test shows the surrounding soft tissues of your shoulder joint. Your provider may order it to look at the condition of the rotator cuff tendons.
Treatment of Shoulder Arthritis
Shoulder arthritis treatments usually begin with nonoperative, home-based, and lifestyle care. These methods keep your shoulder mobile and reduce pain. These treatments include:
- Shoulder exercises: Stretching exercises help improve or retain your range of motion. Your provider may have you work with a physical therapist.
- Activity and lifestyle adjustments: Let pain be your guide. Cut back or avoid everyday activities (for example, lifting heavy objects) or athletic activities that cause shoulder pain.
- Ice and heat: Apply ice or moist heat — whichever feels better — to reduce inflammation and ease your pain. If cold is your choice, place a reusable frozen cold pad or even a frozen bag of peas on your shoulder. Apply the cold pack for 20 minutes at a time, several times a day as needed. Moist heat is a nice option for warming up before stretching or any other time that helps make you feel more comfortable.
Medications
Medications relieve pain and reduce inflammation. Common options are:
- Over-the-counter medications: For short-term pain relief, common choices are acetaminophen (Tylenol®) or a nonsteroidal anti-inflammatory drug (NSAIDs), such as ibuprofen (Advil®, Motrin®) or naproxen (Aleve®). Take only the dosage recommended on the product label or by your provider. High dosages or long-term use can irritate your stomach or cause liver or kidney problems. Never hesitate to contact your provider if you are having side effects. If you need a stronger or longer-lasting medication, talk with your provider. They may order a prescription NSAID.
- Injections: The most common option is an injection of a corticosteroid. Your provider injects the medication into the joint space in your shoulder. Cortisone relieves pain by reducing inflammation in the joint. Because its effects last a few months, you may need several injections during the year.
Shoulder surgery
If other treatment methods don’t relieve your pain and your arthritis is getting worse, surgery may be an option. Common surgical options include:
- Total shoulder replacement surgery: In this surgery, plastic and metal replace the diseased sections of bones in your shoulder joint. Your surgeon removes part of the “ball” of your humerus head. It’s replaced with a new metal head that attaches to a metal stem that goes inside your humerus bone. A smooth plastic socket covers your shoulder socket.
- Reverse total shoulder replacement surgery: In this surgery, your surgeon reverses the location of the ball and socket. A metal head attaches to your shoulder blade and a socket attaches to your humerus.
- Arthroscopic shoulder debridement: In this surgery, small tools and a camera are inserted through small incisions in your shoulder. Your surgeon removes loose fragments of damaged cartilage in your shoulder joint. They also file down bone spurs (if present). This may be an option if you have early arthritis with some cartilage left. Although this procedure doesn’t stop arthritis, pain relief may last up to 24 months.
- Resection arthroplasty: This is the most common surgery for arthritis in the acromioclavicular (AC) joint. In this surgery, your surgeon removes a small amount of bone from the end of your collarbone. The space between your collarbone and shoulder blade fills in with scar tissue.
Glucosamine or Chondroitin Supplements for Shoulder Arthritis
Some people who have arthritis say that glucosamine and chondroitin help relieve their joint pain. These personal reports are hard to evaluate. The Food and Drug Administration doesn’t regulate supplements. Unlike medications, there’s not a lot of scientific evidence to confirm that supplements help treat arthritis.
Prevention of Shoulder Arthritis
We can lower the chances of developing arthritis, in general, by:
- Avoiding tobacco products. If you use tobacco products, your provider can give you tips to quit and offer information on support services.
- Doing low-impact, non-weight-bearing exercise.
- Maintaining a healthy body weight.
- Eating a healthy diet.
- Reducing the risk of joint injuries. Avoid or limit activities that put our shoulders at risk of injury.
What is a frozen shoulder?
Frozen shoulder, also called adhesive capsulitis, is a painful shoulder condition. Like shoulder arthritis, both conditions involve pain and loss of motion in your shoulder.
A frozen shoulder occurs when the strong connective tissue surrounding the shoulder joint (called the shoulder joint capsule) becomes thick, stiff, and inflamed. Even without treatment, a frozen shoulder gets better on its own. This may take from a few months to a couple of years.
Shoulder arthritis doesn’t get better on its own. Arthritis attacks the shoulder joint itself, not the surrounding joint capsule.
 MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka
MATCDHAKA – Medical Assistant Training Centre in Dhaka Pharmacy, Veterinary, Dental, Nursing, Pathology, Physiotherapy and Homeopathy Training Institute in Dhaka